The defect in the mid-facial region results in significant facial disfigurement, presenting a considerable challenge to healthcare providers aiming to restore the patient’s normal facial form and appearance. A well-designed prosthesis not only improve the patient’s aesthetic appearance but also enhance their self-esteem and quality of life. This case report discusses the rehabilitation of a 38-year-old male patient with a mid-facial defect using an adhesive-retained silicone prosthesis. The prosthesis was fabricated using Room Temperature Vulcanizing (RTV) silicone material, carefully matched to the patient’s skin tone and incorporating intrinsic colours. The prosthesis was secured to the patient’s face using a Silicone-based tissue adhesive, resulting in an outcome that was well-received by the patient.
Key words: Mid-facial Defect, Adhesive, Silicone
Mid-facial defects refer to defects in the mid-line
of the face, including the nose and upper lip, as
well as defects on the sides of the face affecting the orbital contents and cheek, either individually or in combination.1
Acquired Mid-facial
defects can cause significant disfigurement and
functional damage. It is essential to seek proper
medical attention and treatment to avoid further
complications.2
Such mid-facial defects that involve intra-oral communication require surgical
reconstruction or a facial prosthesis for management.3
Modern dentistry has introduced several
innovative surgical reconstruction techniques.
However, the field still entails a significant challenge. It is crucial to restore lost structures’ intricate three-dimensional anatomy and morphology while ensuring they are properly covered,
lined, and supported. This often requires the use
of a multi-stage technique and the availability
of healthy local tissue. Facial prostheses can be a better option than surgical reconstruction for
those seeking to restore both the form and function of their face after cancer removal. With their
ability to provide a natural look and feel, facial
prostheses can be a more comfortable and less
invasive solution. Hence, facial prostheses can
be considered to improve your quality of life and
regain confidence.4,1
Fabricating an extra-oral prosthesis can be a
challenging task that requires a great deal of
creativity from the Prosthodontist. The choice of
material for the prosthesis depends on several
factors, such as the need to engage undercuts,
the mobility of the tissue bed, the size of the defect, and the weight of the prosthesis. Due to
the size and weight of the prosthesis, achieving
adequate retention is often a matter of concern
and can be difficult to achieve. Thus the use of
medical grade adhesives, resilient attachments,
clips, and Osseo-integrated implants have been
adopted to properly retain prostheses. These
prostheses can also be connected to an obturator using magnets, spectacles, or headbands.5
In this case report, we describe the rehabilitation
of a 38-year-old male patient with a percutaneous mid-facial defect using a Silicone prosthesis
that is retained with adhesive.
A 38-year-old, male patient reported to the department of Prosthetic Dentistry, with a large defect on the right lateral lower side of the face. His
chief complaint was the inability to chew or drink
due to the leakage of food through the defect.
A detailed case history revealed that the patient
was diagnosed with squamous cell carcinoma
of the right buccal mucosa of the lower lip 20
years ago. The patient had undergone surgical
removal of the right buccal mucosa, and lower
lip, also undergone Segmental mandibulectomy
along with left neck dissection level I - III and
reconstruction with fibula flap along with tracheostomy under general anaesthesia was followed by a course of chemo radiation. The healing of the surgical site was uneventful and stable
for the following 3 months. After three months
during follow-up, the patient presented with a
recurrence of the tumor and underwent composite resection with a Pectoralis major myocutaneous flap (PMMC) in which a 2X2 cm skin defect
was covered with FTSGs Full-thickness skin graft
(FTSGs). After one month patient developed flap
necrosis & and underwent a forehead flap. After
that patient complained of trismus & and cosmetic deformity so he was referred to the Amrita Institute of Medical Sciences. There was a
loss of facial contour on the left side. The skin
on the margins of the defect appeared irregular. The patient was concerned about the defect
and loss of facial contour. He lacked self-esteem
and avoided social interactions due to facial
disfigurement. As surgical reconstruction of the
defect was not possible due to a history of graft
rejection, Prosthetic rehabilitation with adhesive
retained silicone prosthesis was planned. This
prosthesis was thought to prevent the leakage of
food, restore the loss of facial contour, and improve the aesthetics and self-esteem of the patient.
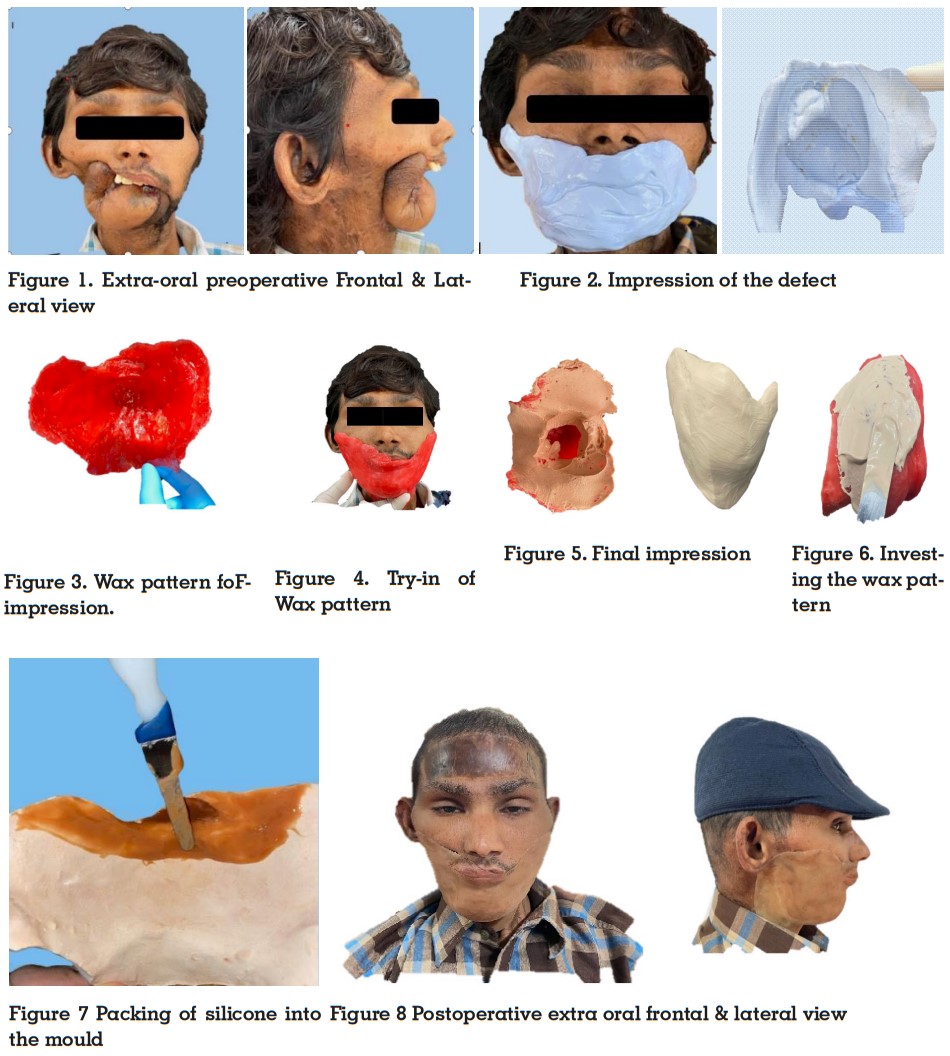
The patient was seated upright in a dental chair
and a facial moulage was made with high viscosity rubber impression (Aquasil) soft putty /
regular set due to severe undercut (Figure 2). After proper beading and boxing, the impression
was poured with type IV die stone and wax up is
done. The defect was outlined on the cast and a
wax pattern was made using modelling wax DPI
products (Figure 3). The trial of the wax pattern
was done on the patient’s face to check the proper seating of the pattern and proper adaptation
of the margins (Figure 4) and with the help of
the wax pattern, the final impression was made
with irreversible hydro-colloid to get the proper peripheral area (Figure 5). The wax pattern was invested in type III dental stone and mould
preparation was done followed by dewaxing
(Figure 6). Processing of the pattern was done by packing the mould cavity with Room Temperature Vulcanizing (RTV) silicone (A-2000, Factor II,
USA) after proper shade matching with the patient’s skin and using intrinsic colours (Figure 7).
Following the proper curing cycle, the final prosthesis was retrieved from the mould, and finishing and polishing were done. The prosthesis was
tried on the patient’s face for proper fit, marginal
adaptation, and colour matching. After a satisfactory trial, the prosthesis was finally retained
on the patient’s face using water-based tissue
adhesive (Probond Adhesive G609, Techno vent,
United Kingdom) (Figure 8). The patient was instructed to apply the adhesive on the margins
of the prosthesis and allow it to dry for 3-5 minutes before applying it to the skin. The prosthesis could be removed using soap and water. The
patient was very satisfied with the final esthetic
outcome.
Large Orofacial defects can result in functional
and aesthetic challenges with significant effects
on patients’ quality of life. This case report describes a patient with a mid-facial defect caused
by a tumour, which significantly affects their
quality of life after surgical removal Prosthetic
restoration of large facial defects is a challenging process, given the lack of anatomic undercuts, restricted means of retention, soft tissue
mobility, size, and weight of the prosthesis.6
To
overcome these challenges, practitioners have
adopted auxiliary retention methods.7,8 Although
Osseo-integrated implants may provide maximum retention of the prosthesis, their large size,
poor mucosal quality, and negligible bony support require supplementary surgical interventions and substantial expenses, which can impact the patient’s long-term prognosis.9
Facial prostheses are typically made from materials such as acrylic resins, co-polymers, vinyl
polymers, polyurethane elastomers, and silicone elastomers. However, none of these materials meets all the essential requirements for
an acceptable prosthesis. Thus the development
of silicone-based prostheses has revolutionized, providing an ideal material that fulfills all
requirements. With its unique properties and
versatility, silicone prosthetics offer a superior
solution for those in need of these life-changing
devices.10
The retention of prostheses used in prosthetic rehabilitation for large mid-facial defects is
determined by their size and weight, which can
make the procedure tedious.11 These kind of defects lead to substantial psychological issues.
In some cases, achieving acceptable aesthetics can jeopardize the retention capacity of the
prostheses. Therefore, attention should be given
to factors such as impression methods, materials used in laboratory trials, prosthesis design,
and connection method, direction of insertion
and/or removal, aesthetic factors, and maintenance protocol. By constructing intra-oral or
extra-oral prostheses that jointly hold each other, proper knowledge of the remaining anatomic structures can be utilized. There are several
techniques for retention for facial prostheses,
including eyeglasses, eye patches, extensions
from the denture engaging desirable tissue undercuts, medical-grade adhesives, magnets,
and Osseo-integrated implants.12,13
In this case-report, patient had a medical history
of undergoing radiation exposure and surgical
intervention for Squamous cell carcinoma of the
right lower lip. Unfortunately, the cancer had recurred and there was also the presence of graft
rejection and fistula of the right mandible. Facial
prostheses are considered the ideal treatment
option for individuals with multiple surgical interventions and large defects in their right lower face, as compared to surgical construction.
The prosthesis in this case was fabricated using
Room Temperature Vulcanizing (RTV) silicone
material (A-2000, Factor II, USA). This material
was chosen because it is easy to customize and
fabricate and has a lightweight, tissue-compatible, and stable design. Additionally, it has both
extrinsic and intrinsic colouring. Various other methods of supporting cheek prostheses are
available, including magnets, headgear, and
spectacles,14 which can enhance the seal and
aesthetics of the patient. In this particular case,
an extra oral prosthesis was provided due to the
irregular size of the defect, loss of facial contour,
lack of self-esteem, and negligible socio-psychological acceptance. The patient expressed good
acceptability and satisfaction with the prosthesis. To ensure successful acceptance and adaptation of prosthetics, good retention, bio-compatibility, and restoration of form and function are
crucial.15
Implant placement was not a viable option in
this case due to the multiple surgical, fistula,
and graft rejection. However, a silicone prosthesis was successfully used instead. The prosthesis was highly retentive, easy to fabricate, and
had impeccable colour matching. Furthermore,
the patient showed great acceptance of the prosthesis.
The surgical reconstruction and rehabilitation of
a significant mid-facial defect present a complex
and fascinating procedure. Fabricating a facial
prosthesis for patients with extensive defects,
who have experienced a loss of self-esteem and
confidence, is a significant challenge and responsibility for the clinician. Unilateral mid-facial defects involving the mandible and cheek,
which are part of the movable structures, often
lack stability unless highly retentive elements or
techniques are employed. In this case report, a
patient experiencing graft rejection recurrence
and a facial defect was successfully rehabilitated with silicone prostheses, leading to favourable
and well-received outcomes. Therefore, it can be
concluded that utilizing facial prostheses made
of silicone material and adhesive technique improves aesthetics, enhances confidence, and elevates the quality of life for patients with severe mid-facial defects.