Rehabilitating maxillectomy defects poses significant challenges that require tailored approaches for each individual patient. To achieve successful outcomes, it is crucial to integrate both traditional and modern treatment methods to enhance the prosthesis’s retention, stability, aesthetics, and functionality. Methods: Three patients with post-COVID Mucormycosis who had undergone localized debridement and partial maxillectomy were treated with a definitive rehabilitation plan. For patients with partial maxillectomy, a cast partial denture designed using Direct Metal Laser Sintering (DMLS) and the altered cast technique was employed. The defect areas were kept as hollow cavities (either closed or open) to reduce the prosthesis’s weight. Results and Conclusion: This approach to prosthodontic rehabilitation proves to be a straightforward and cost-effective treatment, significantly enhancing stomatognathic functions and overall quality of life for patients. Major challenges during rehabilitation include achieving retention and stability due to the absence of basal seat and hard tissue support. To address these challenges, a combination of conventional and digital techniques was utilized to ensure precise fitting and accuracy of the prosthesis, thereby minimizing treatment time and the number of patient visits.
Key words: cast partial denture, mucormycosis, obturator, rehabilitation, altered cast technique
Maxillofacial prostheses aim to restore the
appearance, function, and structure of facial
areas affected by congenital issues, trauma, or
cancer. This specialized field requires extensive
knowledge of dental materials and technologies
to produce long-lasting and effective prostheses.
Following a maxillectomy, which involves the
removal of part of the maxilla, patients face
significant challenges such as difficulties
with oral function, speech, and appearance,
including issues like hyper nasal speech, nasal
regurgitation, and problems with chewing1.
Restoring function with prostheses involves
overcoming challenges such as limited mouth
opening, undercuts in the defect, and obstruction
from the defect’s lateral walls. It’s crucial to
avoid overloading any remaining teeth and to
ensure that the prosthesis remains stable and
functional2. Different obturator designs, including
hollow bulbs and two-piece systems, can affect
the prosthesis’s weight and effectiveness. The
process of prosthetic rehabilitation typically
involves several stages. Initially, a surgical
obturator is used and adjusted to match the
changing defect and surrounding tissues. An
interim obturator assists with oral functions
during the healing phase, until the defect is
stable. Once stabilized, a permanent obturator
is fitted for long-term use3. The prosthesis must
create a secure seal to prevent nasal leakage.
Proper support, retention, and stability are
essential, influenced by factors such as the
defect size, the condition of supporting palatal
shelves, and the state of remaining teeth, which
can act as abutments to improve stability.
Effective
rehabilitation demands thorough
preoperative planning, teamwork between the
surgeon and prosthodontist, and advanced
impression techniques.4 Traditional impression
methods often struggle with these large defects
due to restricted mouth opening and undercuts.
The altered cast technique can address these
issues, enhancing the fit and functionality of
the prosthesis5. This case series focuses on the
prosthodontic rehabilitation and creation of a
hollow bulb obturator for a partially edentulous
patient with an acquired defect, employing
Direct Metal Laser Sintering (DMLS) and the
Altered Cast Technique.
A 70-year-old male with hypertension and non
insulin-dependent diabetes presented to the
Department of Prosthodontics at Government
Dental College, Trivandrum, complaining
about an ill-fitting acrylic maxillary obturator.
The patient reported issues including poor
retention, instability, leakage, and food
accumulation under the obturator, prompting
him to seek a replacement. The patient’s
medical history revealed that he had undergone
a left partial maxillectomy two years ago due
to mucormycosis of the maxilla, which followed
a COVID-19 infection. Extraoral examination
showed facial asymmetry with a collapsed
cheek and a pronounced nasolabial fold on the
left side. Intraoral examination indicated that
the residual maxillary defect had completely
healed. There was visible oro-antral and oro
nasal communication on the left side due to the
partial maxillectomy. Missing teeth included
21, 22, 23, 24, 25, 26, and 27, and the alveolar
ridge was absent with obliteration of the labial
and buccal vestibule on that side. The defect
was classified according to Aramany’s class 1
system. In the mandible, all teeth were vital but
showed generalized physiological attrition.
A 38-year-old male patient was referred from the
Regional Cancer Centre, Thiruvananthapuram,
to the Department of Prosthodontics,
Government Dental College, Trivandrum, for
prosthetic rehabilitation of a maxillectomy
defect. The patient had undergone surgical
maxillectomy 8 months back for the treatment
of mucormycosis. The chief complaints reported
by the patient were nasal regurgitation of food
and fluids while eating along with difficulty in
speaking. An extraoral examination revealed
facial asymmetry, with a lack of support for the lips and cheek on the left side. Mouth opening
of the patient appeared normal, with defective
hypernasal speech. The patient was wearing an
ill fitting interim acrylic obturator that required to
be changed. Examination of the interim obturator
found it to be grossly under sized compared to
the defect itself. Intraoral examination revealed
an Aramany type III palatal defect involving
the left side of the arch crossing the midline.
Intraoral examination revealed the presence of
the remaining natural teeth (13,14,16,17,18) in
the maxilla. In the mandible posterior teeth were
missing and maxillary molar was root canal
treated and capped. The osteomucosal-bearing
surface showed a moderate deep palate and
covered with a thick, adherent fibro mucosa. On
the left side, an existing surgical maxillary defect
with adequate healing was noticed in the hard
palate. This defect was connecting the oral cavity
to the left maxillary sinus and the nasal fossae.
It also presented two moderately deep anterior
and posterior undercuts. The radiological
examination panoramic radiography confirms
the existence of the maxillary defect.
A 45-year-old male patient presented to the
Department of Prosthodontics and Crown &
Bridge at Trivandrum with complaints of missing
teeth, difficulty chewing, drinking, speaking, and
facial deformity resulting from partial maxillary
resection. His medical history was otherwise
unremarkable. The treatment report indicated
that he had undergone resection of the maxillary
ridge, extending from the right lateral incisor to
the left first premolar, 12 months prior due to post
COVID mucormycosis. Extraoral examination
revealed a Class 3 skeletal base with the vertical
dimension preserved. Intraoral examination
showed an Aramany Class VI maxillectomy
defect, resulting in inadequate lip support and a
depressed nasolabial fold. The patient had been initially rehabilitated with an interim obturator
and need to get replaced. All mandibular teeth
were found to be vital.
The patient’s diagnosis includes an acquired
palatal defect resulting from surgical removal
and associated tooth loss. The primary objective
of the treatment was to close the communication
between the oral and nasal cavities with an
obturator, thereby addressing issues related
to speech, swallowing, and deglutition.
Additionally, the treatment aimed to improve
both the aesthetics and functionality of the
patient’s oral cavity.
The proposed treatment plan involved several
steps: providing oral health instructions (OHI),
performing supra- and subgingival scaling
and polishing, offering advice on floss and
interdental brush use, recommending a
fluoridated mouthwash containing 0.05% sodium
fluoride (NaF), and suggesting a toothpaste
with at least 1350 parts per million (ppm) of
fluoride. After these interventions, the plan was
to rehabilitate the patient with a removable
cobalt-chrome partial obturator for the maxilla
using an Altered Cast impression technique and
Direct Metal Laser Sintering (DMLS) fabrication
method, as well as a conventional removable
partial denture (RPD) for the missing teeth in the
mandibular arch.
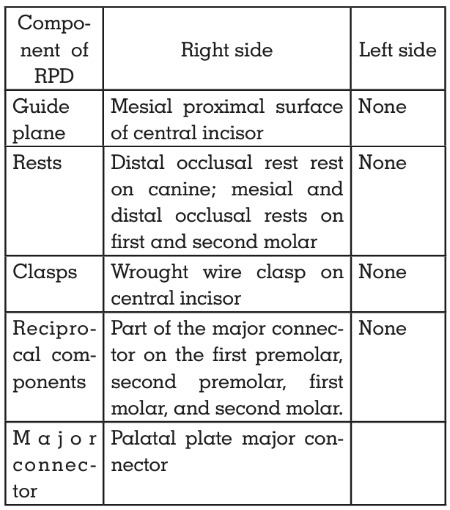
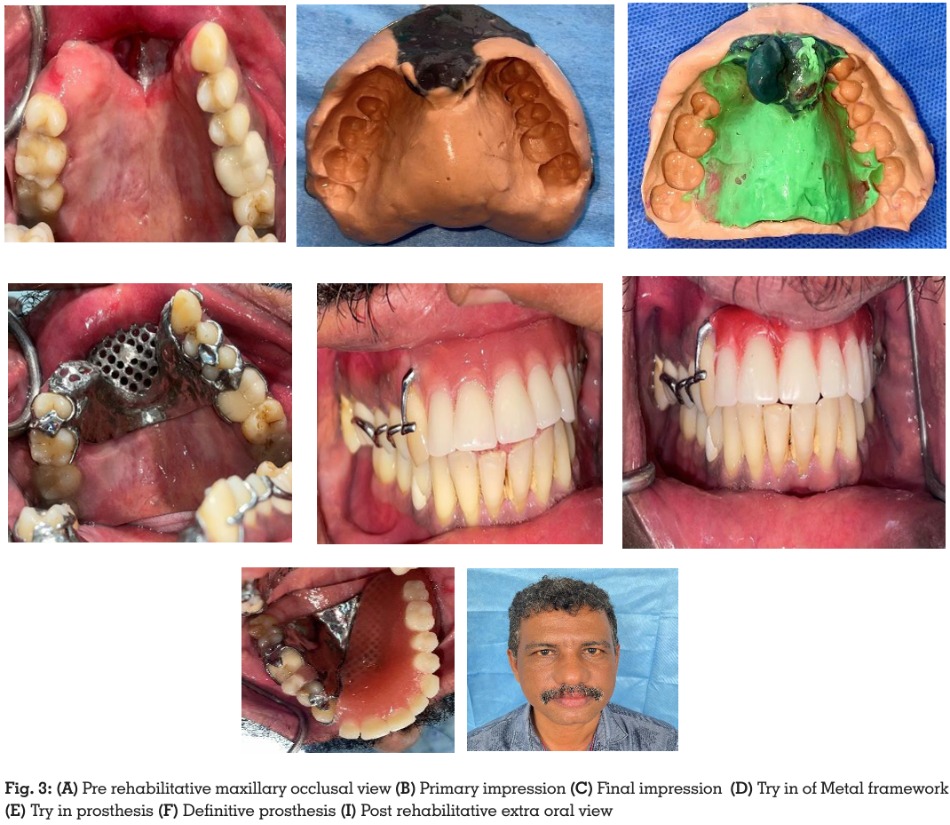
Design for the cobalt-chrome removable partial
obturator (Case report:1)
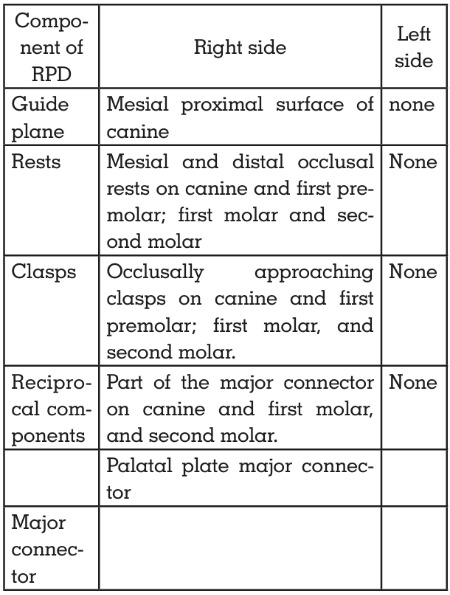
Design for the cobalt-chrome removable partial
obturator (Case report :2)
Design for the cobalt-chrome removable partial
obturator (Case report:3)
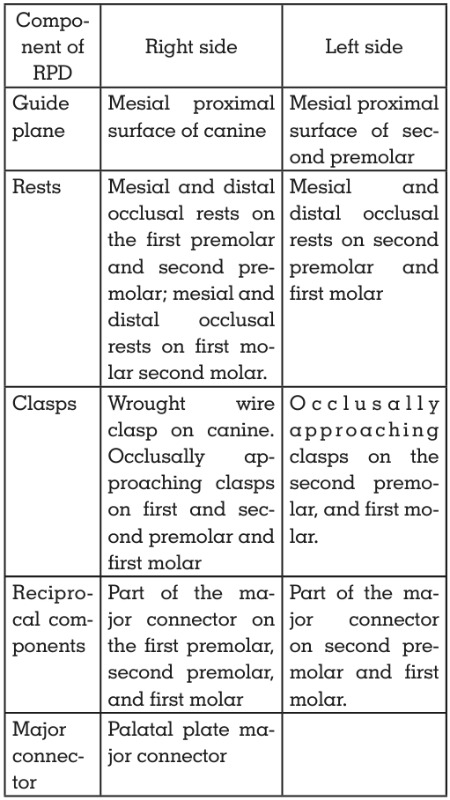
In all cases, primary impressions were taken
using conventional impression techniques
since patient’s had normal mouth openings.
Before taking the impression, any undesirable undercuts were blocked with gauze coated in
petroleum jelly to protect the defect area. An
impression was made using irreversible fast
setting hydrocolloid (AlgitexR) after modifying
the upper stock tray for a better fit and blocking
undercuts with the petroleum-laden gauze.
These impressions were then poured with dental
stone type IV (dfine) to create study models.
The maxillary cast was duplicated for future
reference. Then the study casts were carefully
surveyed to design the metal framework.
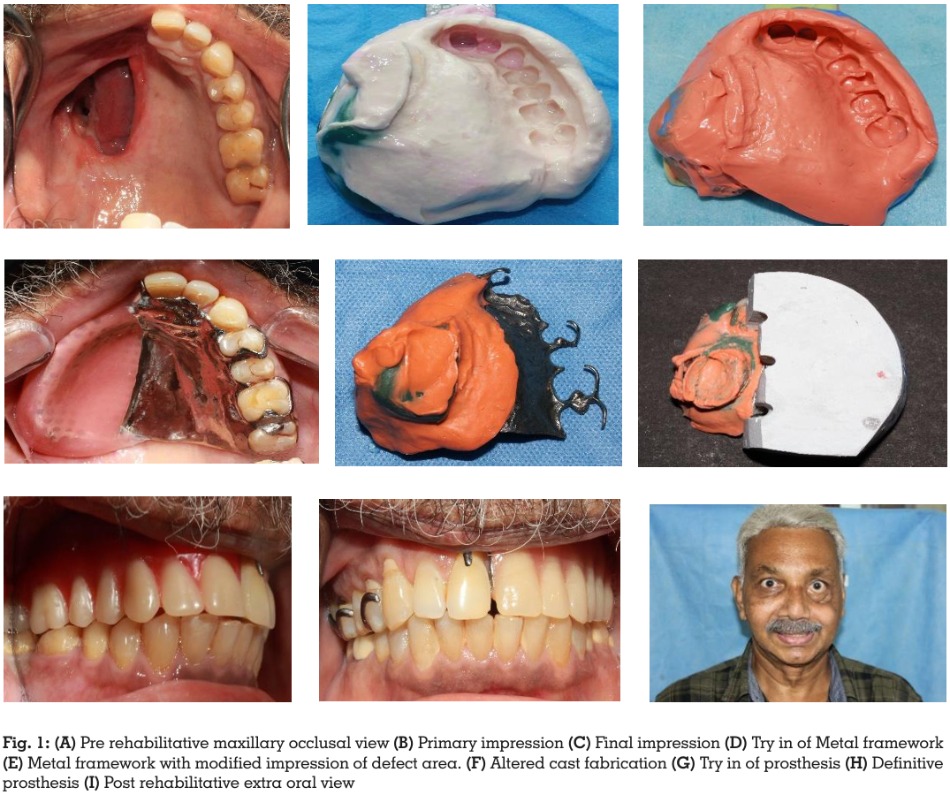
Considering functional and aesthetic needs,
a removable cobalt-chrome partial obturator
for the maxillary arch was planned. Mouth
preparation involved creating a special tray
using cold-cure acrylic resin (Pyrax Rapid
Repair), performing border molding with green
stick compound (DPIR pinnacle tracing stick),
and taking the final impression with polyvinyl
siloxane (PVS) material ( Perfit elastomeric
impression material). The impression was poured
with extra-hard type IV dental stone (dfine, Type
IV Dental Stone) to obtain the master cast, which was then duplicated to create a refractory cast
from investment material.
The master cast was then scanned using shining
3d Autoscan Ds-Ex C Pro Lab Scanner and the
metal framework was designed using CAD
(EXOCAD) and fabricated with Direct Metal
Laser Sintering (DMLS) technology (EOSINT
M270, Germany), enhancing accuracy and
precision. The fit of the framework was assessed by placing it in the patient’s mouth and using a
pressure indicator paste. The master cast was
modified by slicing it on the defect side, inverting
the metal framework with the defect impression
onto the cast, and pouring after beading and
boxing. Once the cast is set, it was removed to
form the altered cast. A denture base using heat
cure acrylic (Acryton-H) was then made on the
altered cast with the framework in place on the
defect side.
Jaw relations were recorded for centric relation,
and the casts were mounted on an articulator.
Teeth selection and arrangement were
performed, followed by a try-in to check for
retention, stability, function, and aesthetics. The
obturator was made in two parts: the bulb and
the lid. An elastomeric index of the defect area
was created, and a 1.5mm thick thermoplastic
resin sheet (Dentmark) was adapted on both
superior and inferior surfaces to form a hollow bulb. The bulb and lid parts were bonded with
self-cure resin (Pyrax Rapid Repair) to create a
single hollow structure. The obturator’s seal was
tested by immersing it in water.
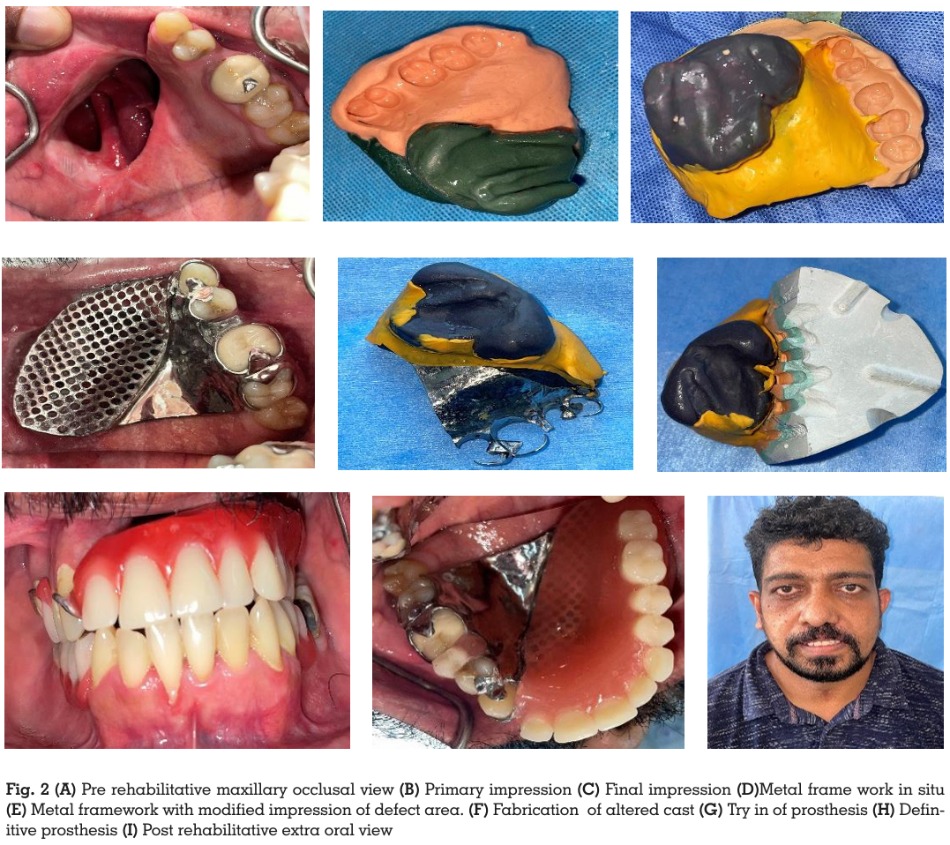
After successful try-in and hollow bulb fabrication,
flasking and dewaxing were carried out. During
packing, the defect area was first filled with
heat-polymerizing acrylic resin (Acryton-H), and
the previously made hollow thermoplastic body
was adapted over it. The entire area was then loaded with heat-cure acrylic resin and cured.
The prosthesis was finished and polished using
standard methods. The following procedures
were followed in all three case reports.
The final obturator was evaluated for fit,
aesthetics, and function. During insertion,
pressure indicator paste (PIP) was used to detect
any excessive pressure points. The denture
was placed in the patient’s mouth, and care
instructions were provided. The patient was
monitored monthly for the first three months and
then every three months for one year, reporting
satisfaction with the improvements in function,
speech, and aesthetics.
Patients who have undergone maxillectomy
often face ongoing challenges in prosthodontic
treatment, particularly issues with support,
retention, and stability of the prosthetic device.
Factors such as the extent of the defect, the
number of remaining teeth, the condition of
the surrounding bone and mucosa, the effects
of radiation therapy, and the patient’s ability
to adapt to the prosthesis all influence the
success of the treatment6. Preserving as many
of the remaining teeth as possible is crucial
for achieving optimal prosthesis design and
functionality. However, a large, heavy obturator
can put continuous pressure on tissues,
potentially affecting tissue health, function, and
comfort.
Retention of the obturator can be achieved
through several methods, including using
remaining teeth, the ridge, lateral aspects of the
defect, undercuts in soft tissue, and scar tissue.
Stabilization and indirect retention components
must be carefully positioned to prevent movement
of the prosthesis over the defect2.
Implant-supported
fixed prostheses are generally not recommended for these patients
because they require periodic removal and
cleaning, which can be challenging given the
secretions from palatal defect areas. Implant
supported overdentures are a better option
but come with higher costs and the need for a
second surgery7. In such cases, conventional
cast partial dentures are often preferred over
acrylic partial dentures. Cast partial dentures
offer superior accuracy, durability, resistance
to distortion, thermal conductivity, cleanliness,
and reduced bulk. Despite these advantages,
cast partial dentures also have limitations, such
as fabrication difficulties, the need for more
equipment, and potential inaccuracies from
manual casting processes2.
To address these challenges, Additive
Manufacturing (3D printing), particularly Direct
Metal Laser Sintering (DMLS), has gained
significant attention in the dental field. This
technology allows for the creation of metal
based appliances with improved accuracy
and precision. The digital workflow provided
by 3D printing offers many benefits, including
shorter laboratory and clinical treatment
times, optimized production steps, reduced
human error, electronic file transfer and
storage, enhanced accuracy, and better patient
satisfaction. Additionally, it allows for finer
details and more precise anatomical features,
resulting in less material waste8. In the present
case series, the prosthetic rehabilitation of partial
maxillectomy patients were performed using
DMLS-designed cast partial dentures. DMLS
is a fabrication process that builds complex
3D structures directly from CAD designs in thin
layers without additional machining, leading
to improvements in fit, function, and aesthetics.
The use of DMLS and other technologies, such
as milling machines, has been shown to surpass
conventional casting methods in producing
metal denture frameworks5.
Various techniques have been developed for
fabricating removable obturator prostheses,
with the extent of the prosthesis dependent
on the ability to accurately record the defect’s
maximum tissue extent. Accurate impression
techniques are crucial for providing stability.
Techniques such as the two-piece impression
technique, custom adapted trays, and separate
defect impressions have been used, but they
may have limitations related to the integration
of the defect into the denture base. The retention
of obturators relies on engaging remaining
teeth or undercuts in the defect, which obstruct
the removal path, particularly on the defect’s
lateral wall. Recording greater depths in a large
maxillary defect helps create a long lever arm
for increased stability and retention. The two
stage impression technique with an altered cast
technique can help overcome many limitations
of previous methods(7).
Heat-polymerizing acrylic resin is commonly
used due to its ease of manipulation, superior
hygiene, color stability, durability, and tissue
compatibility. It contributes to the lightweight
nature of the prosthesis, which helps in cantilever
mechanics, minimizes soft tissue burden,
and enhances speech resonance. The bulb
component of the obturator is often hollowed
out to reduce weight, which can decrease
the prosthesis’s overall weight by up to 33%,
depending on the defect’s extent9.
The design of the obturator framework should
follow fundamental prosthodontic principles,
including stress distribution over a broad
area, use of a rigid major connector for cross
arch stabilization, and strategic placement
of stabilizing and retaining components to
minimize displacement due to functional forces.
It is essential to wait for the defect site to fully heal
and stabilize before constructing the definitive
obturator, typically between 3 to 6 months post-surgery, depending on various factors such as
tumor prognosis, defect size, healing progress,
and tooth presence3.
Improving the quality of life for hemi maxillectomy
patients is more challenging compared to those
with conventional prostheses. However, with
expertise, knowledge, and experience, specialists
can achieve significant improvements. A team
approach, leveraging skills and experience
at
each stage of treatment, and regular
patient evaluations can effectively address the
challenges faced by hemi maxillectomy patients.
The primary challenge in a maxillectomy patient’s recovery is ensuring adequate retention, stability, and support. A thorough understanding of the patient’s needs and extensive expertise is critical in effectively rehabilitating these individuals(10). The patient’s masticatory abilities, speech intelligibility, and overall quality of life can be significantly improved by designing a definitive obturator prosthesis with maximum coverage and appropriate design.
Conflict of Interests Statement
The authors declare no conflicts of interest.
Consent and Ethical Clearance
As per international standard or university
standard, patient’s written consent has been
collected and preserved.