Aim:-To outline the evidence on the use of pterygoid
implants in the rehabilitation of atrophic maxilla.
Methods:- A comprehensive electronic search in
PubMed and Google scholar was carried out to
screen relevant articles based on title, abstract, and
full text published in English language between
January 2013 and June 2023. Studies assessing the
clinical outcomes, survival rate, complication of
pterygoid implants when used in atrophic maxilla
were eligible for this review while studies focusing on
the ideal length, angulation for implant placement,
letter to editors, review articles, short communications
and conference proceeding were excluded.
Results:- A preliminary search yielded a total of 28
studies through search strategy used in Pub Med
and Google Scholar. After screening, six articles
were included for qualitative synthesis while
the remaining articles were excluded for being
duplicates, virtual studies, focusing on parameters
other than the predefined objectives of this review,
and not providing relevant data. The survival rate
in the included studies ranged from 88.06% –100%.
The clinical outcomes reported were probing depth, sulcus bleeding, and plaque. The marginal bone
loss ranged from 0.28–1.21 mm. Post-operative
complications like mucositis, fractured prosthesis,
chipping of ceramic, peri-implant mucositis, and
mobility, bleeding or discomfort were observed in
1.02% (13 of 1,279) of the patients.
Conclusion:- The survival rate of pterygoid implants
when used in an atrophic maxilla is high. These
implants lead to a minimum marginal bone
loss. Further, the complications associated with
pterygoid implants are also minimal with no clinical
significance.
Key words: pterygoid implant, atrophic maxilla, rehabilitation, survival rate, complications
An increase in advancement in the field of medicine and science, there is an increase in the lifespan observed in the population. However, along
with this benefit, the old age diseases have also
become prevalent.1 According to the Global Oral
Health Status report of World Health Organization 2022, the estimated global prevalence of
complete edentulism in people above 20 years
was around 7% while the rate reaches 23% for
people aged 60 years and above.2
Dentures and
bridges still remain the traditional way of rehabilitating loss teeth. However, the advances in
treatment i.e., the use of dental implants have
shown a remarkable increase in the last 30 years
owing to its high success rate.3 The10-year survival rate of dental implants is estimated to be
96.4%.4 Moreover, the complications associated
with dental implants are also reported to be low.5
Based on the relationship of implants with the
oral tissues; the endosteal, subperiosteal, and
transosseous implants are the three major categories of implants.6 Per-Ingvar Branemark’s theory of osseointegration expanded the range of
restorative options for patients who were either
partially or completely edentulous. Osseointegration is explained as a direct functional as
well as structural connect between the surface of osseous implant and the living bone.7 It thus
allows for a new bone formation around its surface thereby forming a fusion and improving the
stability and success rate of the prosthesis. For
osseointegrated implants, the 4–9 years success
rate was 89.06% for individual implant while
100% for prosthetic treatment.8
Dental implants continue to have a certain percentage of implant failures despite a steady rise
in their success rate. Poor bone quality, infection that impedes primary bone healing, and a
lack of primary stability due to trauma during
surgery, are some of the local causes of implant
failure whereas, corticosteroids, uncontrolled diabetic mellitus, collagen abnormalities, bisphosphonate medication, and osteoporosisare other
systemic diseases that affect the early stages of
bone regeneration. It is to be noted that, apart
from these causes, the site at which the implant
is placed also hold a great importance in the
success of prosthesis.9
and for the same reason; there are still certain limitations to implant success in maxillary posterior region compared to
anterior region. The posterior maxilla presents a
biological and anatomical challenge due to its
proximity to the maxillary sinus and its reduced
residual bone volume after tooth loss combined
with poor bone density.10 This is especially true if
the tooth loss happened years ago. As a result, it
has long been difficult to use dental implants to
reconstruct the atrophic posterior maxilla.
Due to the paucity of bone in these individuals, additional/conventional implants frequently cannot be placed without first augmenting
the hard tissue. The literature has documented
many augmentative procedures, with the use of
xenografts, alloplastic, autologous, and allogenic materials. However, all these procedures require a healing period prior to placement of the
implant and also have a high risk of complete
or partial loss of graft along with significant invasiveness.11 Zygomatic implants and all-on-4
implants were also introduced; these too presented complications of graft displacement into the sinus cavity, perforation of sinus cavity, and
loosening of screws of the implants.12 In these
scenarios, the researchers proposed placing implants on the posterior most part of the maxillary tuberosity and area distal to the maxillary
sinus.13 The availability of thick cortical bone for
engagement of the implant is the main justification for employing pterygoid implants. Additionally, it aids in avoiding the necessity for surgeries to raise and graft the maxillary sinus. This
might cut down on treatment time and enable
immediate pterygoid implant loading. Further,
it enables a prosthesis to have enough posterior extensions, which eliminates the necessity for
cantilevers at the distal end.14
Nevertheless, pterygoid implant also demonstrates complications like risk of damage to the
proximal structures during implant placement,
technique sensitivity, difficulty in access to the
posterior most regions of the maxilla, and a slow
learning curve.14 So far few systematic reviews
have been conducted on pterygoid implants.15,16
However, since last reported review, new studies have been published on pterygoid implants in
atrophic maxilla providing a better knowledge.
This systematic review was thus conducted with
a focused question of: What are the clinical outcomes and success rate of pterygoid implants in
atrophic maxilla?
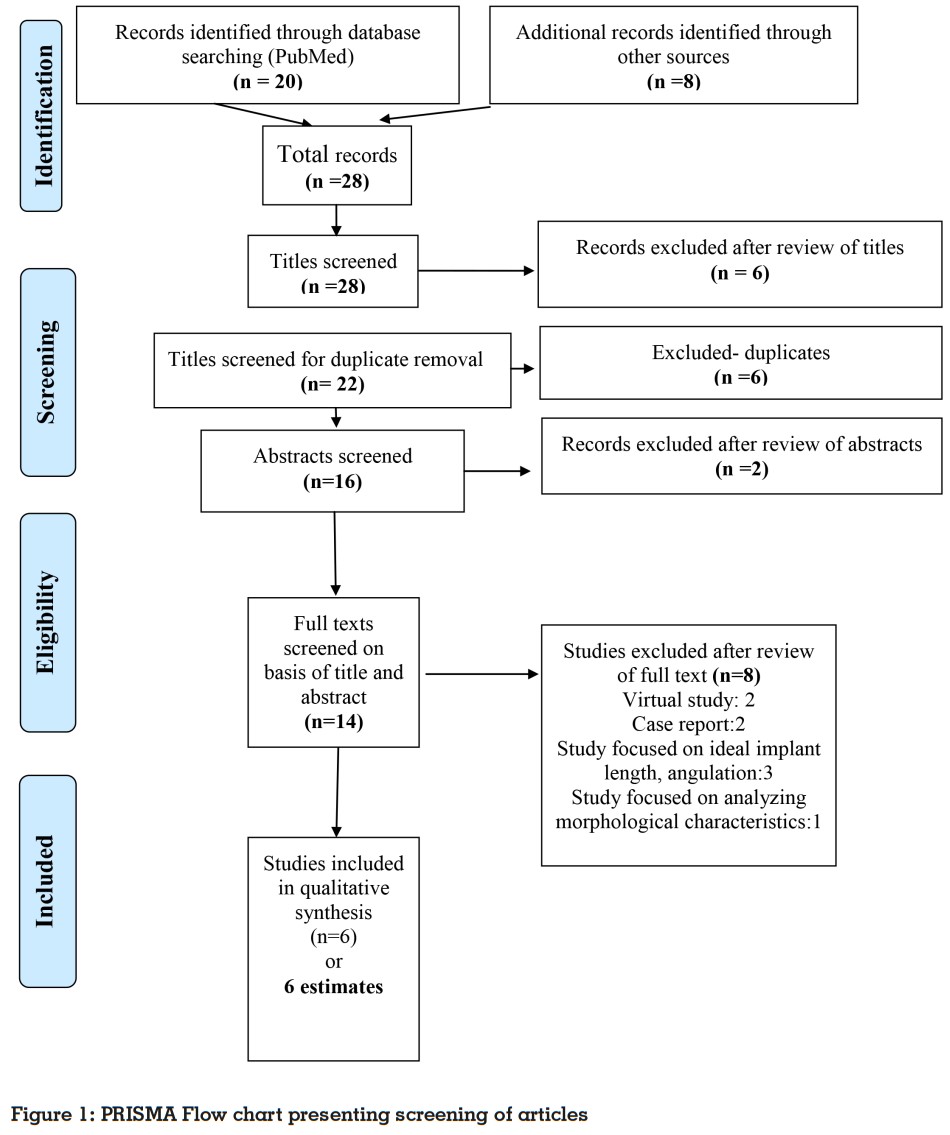
The current systematic review was conducted
and written according to the Preferred Reporting
Items for Systematic Reviews and Meta-analyses (PRISMA Statement) checklist Recommendations and is registered with no. CRD42023435414
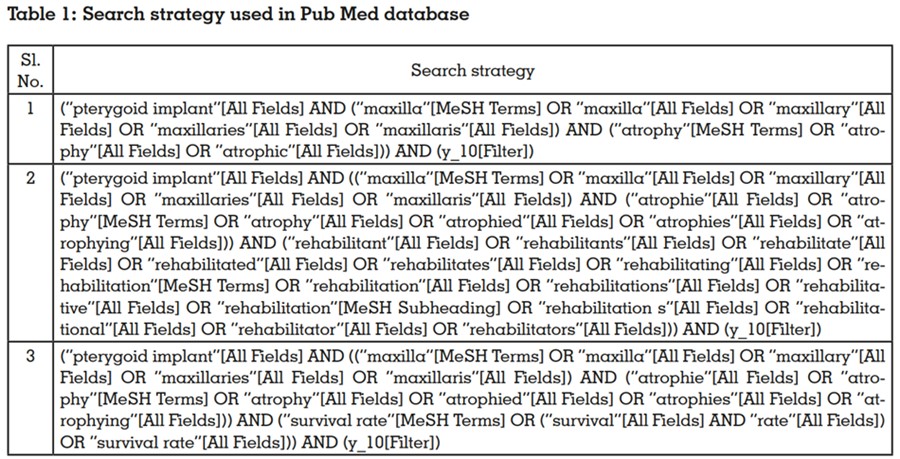
Both PubMed and Google Scholar were searched
in-depth for the data. The search strategy in the
database was developed utilising Boolean operators, controlled vocabulary (MeSH terms in
PubMed), and free-text terms and phrases in
the titles and/or abstracts linked to pterygoid
implants and atrophic maxilla. In Table No. 1,
a thorough search method for PubMed is described. The best match option and the publication date were selected as the filters. In addition
to looking through search results, publications
were identified through exploring cross references within the selected study and browsing specialist journals for pertinent content.
Point of Relevance:-
The PICO (P: patients with atrophic maxilla, I:
pterygoid implants placed in maxilla, C: this review did not aim to compare the pterygoid implants with other implants thus no comparator
or any comparator as implants was considered,
O: survival rate, clinical outcomes, complications) based eligibility criteria included studies
reporting clinical outcome and/or survival rate
of pterygoid implants in pterygomaxillary region
irrespective of any follow-up, number of patients,
and size and diameter of the implants included.
Study designs considered were prospective cohort studies, retrospective cohort studies, and
randomized controlled studies published in English language between last 10 years (search
conducted in June 2023) were included in the
review whereas studies reporting data through
animal studies, laboratory studies, cadaver
studies, in-vitro studies, radiographic studies focusing on standard implant length r technique
were excluded. Along with this, the reviews, editorials, conference proceedings were also excluded from this review.
The titles and abstracts acquired through the
search technique were independently reviewed
by one review author (Dr. Neelam Pande), who
then included them in accordance with the eligibility criteria. The entire texts of all the studies
that had been included were then obtained and
read in order to make a final decision on their inclusion. The second author (Dr. Anushree Bhoge) was consulted in order to clarify any uncertainties regarding study eligibility.
A standardized data extraction form known
as a ‘pilot form’ was created in Microsoft Excel
Spreadsheet with an expert’s guidance. The
form included details on the study variables
like; authors, publication year, study design,
sample size, patient’s age, implant manufacturer, follow-up period, evaluation method, and
study outcomes like; success rate, probing depth
around the implant, modified sulcus bleeding index, plaque index, marginal bone loss, complications, reason of implant failure, and inference
by the study author. Data was initially retrieved
from two papers and presented in a pilot sheet,
which was then approved by an expert to proceed with additional data extraction. Any disagreements between the authors were settled
through conversation.
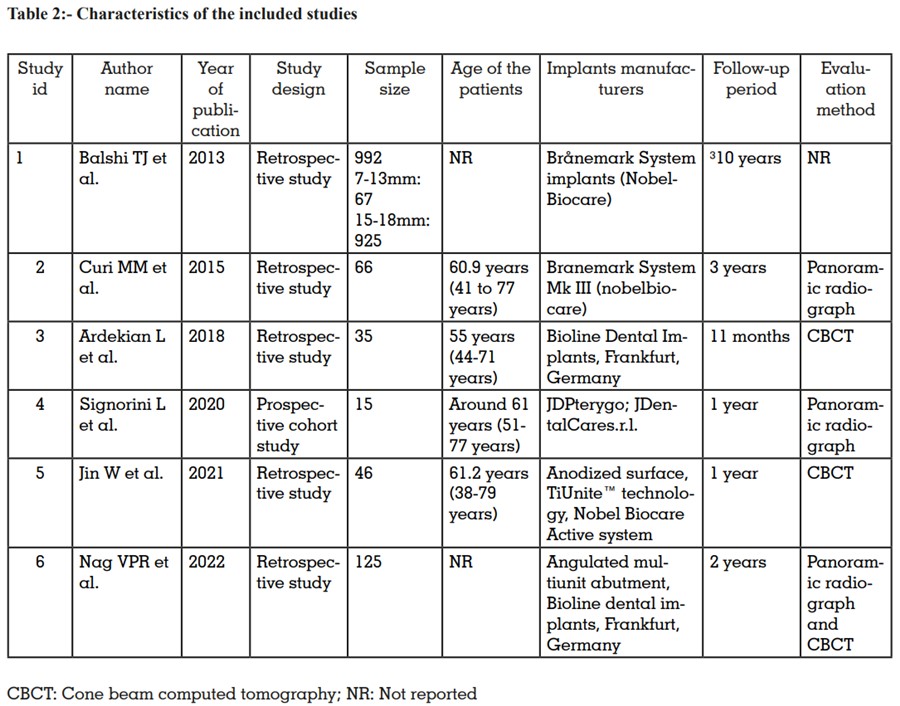
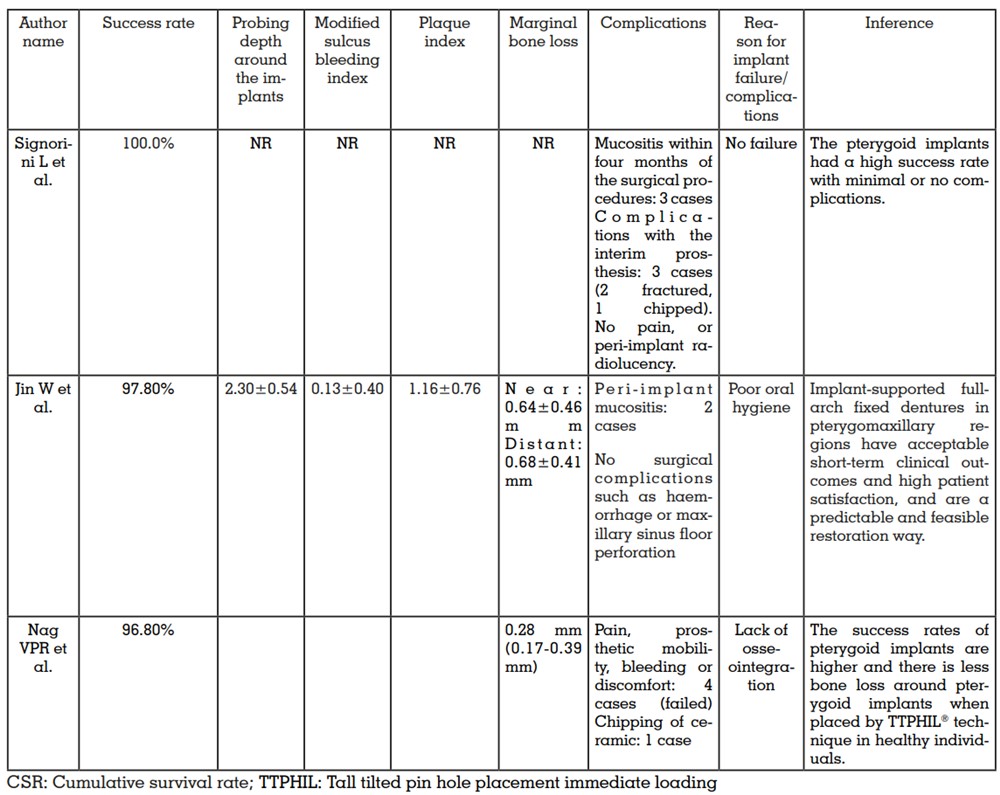
The database search identified 28 studies of
which 20 were from PubMed search while eight
articles were from Google scholar search. After
screening of titles, six studies were excluded and
further another six studies were excluded as they
were duplicates. The remaining 16 studies were
screened based on abstract of which two studies were excluded as the abstract confirmed the
studies to be non-eligible for the review. The full
texts of remaining 14 articles were read and a
total of eight articles were excluded at this step
due to reasons: virtual study (n=2), case report
(n=2), study focused on ideal implant length and
angulation (n=3), and analysed morphological
characteristics (n=1) keeping the final count of
six articles.17-22 The characteristics of the included studies are presented in Table 2. The studies
presented the below outcomes.
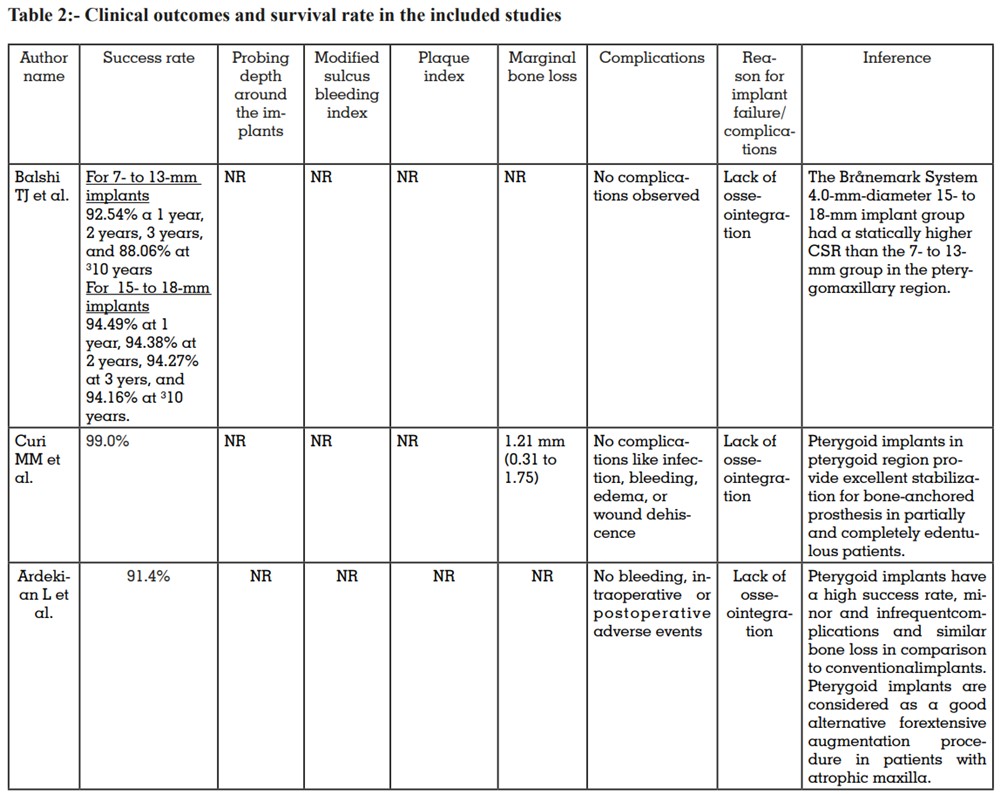
A high survival rate was reported in all the six
included studies of this review. The survival rate
ranged from 88.06% –100% with a mean follow-up between 11 months–10 years. The success
rate was high in the initial years but decreased
with the advancing years and was reported to be
lowest (88.06%) at a follow-up of more than 10
years. In all the cases of failure, the major reason was lack of osseointegration.
The mean probing depth around the implant
was 2.30±0.54 mm, sulcus bleeding as recorded by modified sulcus bleeding index was
0.13±0.40, and plaque recorded by plaque index was 1.16±0.76. These parameters were reported in only one study. The average marginal bone loss after placement of implant ranged
from 0.28–1.21 mm.
Majority of the studies reported no complications
like infection, edema, or wound dehiscence,
bleeding, intraoperative or postoperative adverse events, pain, implant radiolucency, haemorrhage or maxillary sinus floor perforation.
However, 13 patients (1.02%) out of 1,279 patients
experienced complications like mucositis within
four months of the surgical procedures (n=3),
fractured prosthesis (n=2), chipping of ceramic
(n=2), peri-implant mucositis (n=2), and mobility, bleeding or discomfort (n=4).
The concept of pterygomaxillary region was introduced by Tulasne in the year 1992.23 By 1989,
Paul Tessier proposed an idea of placing implants in the ptegomaxillary region considering
the failure of various techniques used in rehabilitation of posterior maxilla.24 According to the authors, posterior atrophic maxilla retains around
80% of the original bone corridor, which is sufficient for placing a long implant.25
Radiographic evaluation of pterygomaxillary
region provides useful information before planning implants in this region. The ideal process
of placing an implant in the pterygoid region is
through pterygoid process into the pterygoid fossa; further, the implants are placed in the middle
part of the pterygoid process as it consist of the
thickest bone for implant support.12,26 Considering their long path into the bone, the length of
these implant ranges from 15mm – 22mm.19,27,28
In the present review, the pterygoid implants
used in the included studies ranged from 7mm
to 22mm.17-22 The results are similar to the previous systematic review that reported the implant
length between 13mm to 20mm.15
The survival rate of pterygoid implants in the
present review was between 88.06% and 100%
at a follow-up ranging from 11 months–10 years
indicating that the survival rate of these implants
was high in atrophic maxilla.17-22 The highest survival rate was observed at 1 year post procedure
while the least was observed at 10 years.17,20 The
primary cause of failure of implants (a small
percentage though) in the included studies was
discussed as lack of osseointegration. However,
none of the studies included in the systematic review reported by Araujo RZ et al. (2019) provided
a reason for implant failure.15 The high survival
rate of the implants can be explained by the
presence of dense bone in the pterygoid region
that promotes osseointegration;29 the implant design which is longer and wider compared to conventional implants thereby providing enhanced
stability and support; a secure anchorage due
to surrounding bone and anatomical structure;30
and a surgical technique which involves optimal
positioning of the implants through an advanced
surgical technique with careful planning and
precise placement.31 Studies have also reported thorough cleaning of the oral cavity during
implant surgery, removal of all necrotic tissues,
and antibiotic therapy for overcoming inflammation as the attributable factors for the success
of implants.20 Nevertheless, it should be noted
that apart from these factors, the survival rate
also depends on patients overall health, oral
hygiene, and adherence to post-operative care
instructions. However, the survival rates in this
review also highlight that they present a steep
decrease with advancement in years.32
The clinical outcomes with respect to pterygoid
implants were not extensively reported in the included studies. Only three studies reported about
the clinical outcomes in terms of probing depth
around the implants, sulcus bleeding, plaque,
and marginal bone loss. The average marginal bone loss after placement of implant ranged
from 0.28–1.21 mm.18,21,22 The minimum bone loss
can be attributed to the implant design, surgical
technique, bone augmentation, and possibility
of immediate loading.
Placing the implants at different angulation rather than straight was observed in the studies included in this review. The implants were placed
in angles ranging from 25°–60°.
17,19-22 These angles are decided based on the height of tuberosity and the floor of maxillary sinus. According
to the literature, tilting the posterior implants allows for the implantation of lengthier implants.
As a result, the contact area between the implant
and the bone expands, improving the implant’s
main stability. The implant support is more distal, and the space between implants is greater
than when straight implants are used, resulting
in a shorter or perhaps non-existent cantilever
length. This improves stress distribution and
optimises the implant’s anteroposterior spread
over the alveolar ridge.33
Although pterygoid implants are a reasonable treatment option in certain cases, they are linked
with potential complications. It should be noted
that the occurrence and severity of complications might vary based on individual patient
characteristics, surgeon ability, and the specific
implant system utilised.34 In the present review,
the included studies reported on the complications in 4% to 40% patients, reportedly; mucositis, peri-implant mucositis, pain, prosthetic
mobility, and discomfort, chipping of ceramic,
and complications with the interim prosthesis.
Nevertheless, these complications were minor
in nature and no major complications like massive bleeding from the maxillary artery or its
branches during the surgery or other that would
cause significant impact on the survival rate of
the implant were witnessed by the authors in
the studies.20,21,22 Further, none of the patients
experienced complication like infection, edema,
bleeding, wound dehiscence, adverse events,
pain, and peri-implant radiolucency in the studies reported in studies by Balshi TJ et al. (2013),17
Curi MM et al.(2015),18 Ardekian L et al. (2018),19
and Signorini L et al.20 (2020) in this review. The
results of this review are in accordance with the
previously reported review.15
None of the studies included in this review had
patients with sinus floor lift or bone grafting.17-22
Pterygoid implants are a treatment option for patients with severe maxillary atrophy, where there
is significant bone loss in the posterior maxilla.
The advantage of pterygoid implants is that they
utilize the available dense pterygoid bone, which
may still be present even in cases of severe maxillary atrophy. By anchoring the implants in this
region, it is sometimes possible to avoid the need
for bone grafting or sinus lift procedures, which
are commonly required to augment bone height
or volume in the posterior maxilla.35 This benefit
also allows rehabilitating patients with satisfactory full arch fixed maxillary prosthesis, which
usually spanned from second molar to second molar. However, it’s important to note that not all
patients are suitable candidates for pterygoid
implants without bone grafting or sinus lift procedures.36 The decision to perform these additional procedures depends on individual patient
factors, such as the amount and quality of existing bone, the proximity of the sinuses, and the
desired treatment outcome. Each case should
be evaluated by an experienced oral surgeon
or implant specialist who will assess the specific
condition of the patient’s jaw and determine the
most appropriate treatment plan.
Before planning implant insertion in the posterior location, radiographic examination of the
pterygomaxillary region is important. According
to studies, panoramic radiographs do not give
required information, and CBCT in implant design may be beneficial in assuring the success
of pterygoid implants. Because of its usage in
pre-surgical planning, CBCT aids in examining all planes and decreases the likelihood of
complication from inappropriate implant failure. Furthermore, as compared to a CT scan, it
exposes patients to less radiation.37,38 However,
it should be noted that the radiographic evaluation of the implants in the included studies of
this review was either done by panoramic radiography or a CBCT with maximum studies evaluating implants via panoramic radiographs.
This indicated that, inspite of the advantages of
the CBCT over panoramic radiography; the preferred choice among the dentists is panoramic
radiograph. The possible reasons may be due
to inability to compare the grey values within the
patient at different intervals or among a set of
patients thereby compromising the assessment
of bone density. Further, the quality of images is
highly influenced by the exposure parameters.39
The review certainly has few limitations. The results of this review come majorly from retrospective studies (low level of evidence) and thus need to be interpreted with caution. The sample size of
most of the included studies was small and the
follow-up was for 1 year to 3 years with only one
study reporting outcomes at 10 years follow-up.
Within the limitations of this review it can be
concluded that the survival rate of pterygoid implants when used in anatrophic maxilla is high.
Thecomplications associated with pterygoid implants are minimal with no clinical significance.
Considering the position and the angled placement of the implants in the jaw, it aids in preventing the need of bone grafting and sinus lift and
yet provides a stable anchorage for survival and
distribution of occlusal load. However, further
studies prospective studies are recommended
wit long term follow-up to assess the evidence
on the survival of the implants with clinical outcomes in a long run.