

Dental implant therapy is by far the closest replacement to natural teeth when compared to other fixed prosthetic alternatives. Aesthetic implant therapy enhances every aspect of oral implantology, thus evolving into a fundamental component of contemporary implant dentistry. Lately, significant advancements have been made, such as the development or regeneration of implant recipient sites through the stimulation of both soft and hard tissues, as well as the replication of sound peri-implant tissue architecture that are resistant to masticatory trauma and mechanical forces. Modern esthetic approaches require patient’s preferences to be taken into consideration, and spontaneous addressal to their specific issues have become inevitable in modern aesthetic implant practice from a restorative sense. This review examines the key historical context surrounding dental implant aesthetics and outlines the various crucial elements that are necessary to guarantee a solid foundation to an aesthetically pleasing implant with stable anchorage. If aesthetic risk factors are to be identified and appropriately managed, then an interdisciplinary, systematic, prosthetically driven approach is required.
Key words: osseointegration, platform switching, guided tissue regeneration.
More than ever, implant dentistry places a strong
emphasis on the patient’s overall appearance,
which improves social interaction as well as the
patient’s sense of self-worth and confidence. This
has resulted in the development of novel loading
concepts, adaptable restorative options, complex
implant designs, innovative, esthetic surgical techniques which are less invasive. As a consequence
of this, dental implants are now employed with exceptional treatment success rates thanks to more
precise surgical and biomechanical protocols. In
other words, these ideas helped usher in a new
era of clinical predictability which is an amalgamation of function with esthetics.
Titanium dental implants, which are used in
contemporary dental care, have been shown
to be secure and efficient in the longevity of esthetic implant therapies in well-controlled, longterm studies. Other dental materials include
hybrid ceramics & zirconia implants. There is
little research to support the general efficacy
and durability of aesthetic therapeutical methods employed in anterior implant rehabilitation
from a prosthodontic purview despite recent developments observed in the practices of many
clinicians. Consequently, for esthetic implant
therapy, a standard surgical and prosthetic
protocol is required.
Cosmetic dentistry has been practiced by ancient civilizations like Egypt for over four millennia. In the region of Central America, fine dark
stones in the shape of teeth were discovered implanted within certain Mayan skulls around 600
A.D., suggesting surgical implants have played
a significant role in the evolution of dentistry in
substituting lost teeth. In 1952, Branemark started the current wave of implant usage. Osseo
integrated implants are now a vital tool in the
restorative dentist’s toolbox for treating patients
who are either completely or partially edentulous, and in addition to function, aesthetics is
given top priority.
Patients are currently considering visible crown
margins or an inaccurate porcelain color match
over an implant-supported prosthesis as an unsatisfactory treatment outcome because contemporary implant dentistry concepts have
progressed beyond basic needs and now must
include aesthetic corrections, a new challenge
that an implantologist must overcome. Achieving this aesthetic is frequently challenging, if not
impossible. Hence this article encompasses an
overview of the contemporary clinical parameters of esthetic implant therapy, principles of the peri-implant architecture including hard and
soft tissue esthetics along with some potential
treatment complications in the aesthetic zone.
In the modern world, achieving optimal implant
aesthetics requires more than one step or process.
To reduce the aesthetic risks associated with dental implants, a thorough esthetic diagnosis must
be made. This involves collecting all the relevant
aesthetic data including the patient’s expectations
regarding aesthetics into account prior to offering
a possible prognosis of an impending implant rehabilitation. Hence performing a thorough esthetic
diagnosis has become imperative to ensure predictable results in the placement of restoratively
driven implants.
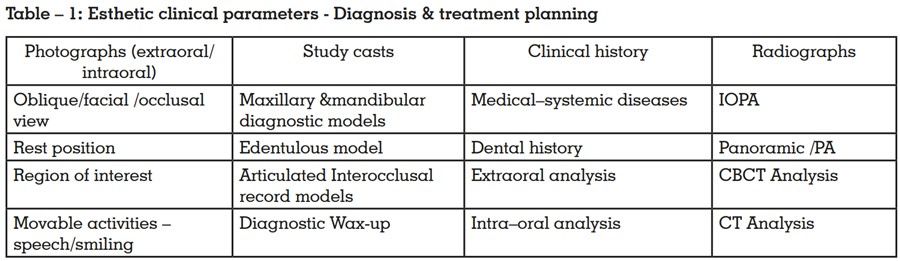
A successful introductory patient visit should
yield a comprehensive clinical record with good
intraoral and extraoral images, screening x-rays
that may reveal potential abnormalities or aberrant anatomy, and flawless study casts. (table-1)
The appearance of an implant restoration can
depend on several factors, such as individual’s
smile line, tooth shape and position, periodontium biotype, size, type of implant and bone
anatomy.
Principles of esthetic therapy:
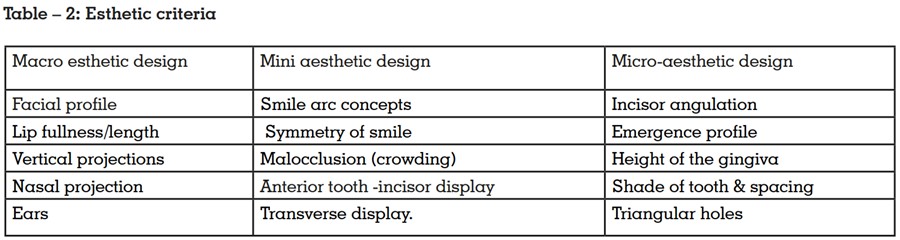
Clinicians’ expanding use of cosmetic restorative procedures has generated greater interest
in the determination of esthetic guidelines and standards1. The esthetic criteria can be broadly
analysed through clinical parameters such as
macroesthetics, miniesthetics, and microesthetics as proposed by Sarver & Ackerman2
(Table
-2)
Precision in implant placement often requires
the tooth positions to be evaluated in apico-coronal, buccal-lingual, and mesio-distal planes, as
3D implant placement has high significance on
the regeneration of gingival architecture.
Hard & Soft Tissue Aesthetics
In an aesthetic zone, rehabilitation in general,
is very technically known for its precision. Consequently, a number of strategies have been put
forth to stop bone loss and maintain the amount
of hard and soft tissue within the intervention
area. Success in implant rehabilitation involves
the following areas: peri-implant hard tissue
augmentative surgery, precision in implant
placement, and peri-implant soft tissue management.
Clinical anatomic site analysis for ideal soft
and hard tissue esthetics should include3
:
Hard tissue aesthetics:
The strategy for achieving hard tissue architecture include employing bone graft materials,
varying implant loading and placement timing
protocols, designing new implants and placing them in particular locations. The proficient
hard tissue augmentation procedures generally
performed include atraumatic tooth extractions,
ridge preservation procedures (bone grafts,
guided tissue regeneration) with immediate implant placement, partial extraction therapies
such as the socket shield therapy, flapless implant surgery, ridge augmentation using autogenous grafts, distraction osteogenesis, etc4. For
reconstruction of the extensive bony defects, autologous, allogeneic or xenogeneic bone graft ing (guided bone regeneration), and the application of biological agents along with growth
factors are conventionally considered5.
Soft tissue aesthetics:
The predictability of the peri-implant esthetic
outcome may ultimately be determined by the
patient’s own presenting anatomy which include
relative tooth position, form of the periodontium, biotype of the periodontium, tooth shape,
and position of the osseous crest6. The most
popular peri-implant soft tissue techniques include: minimally invasive techniques that cause
less tissue trauma; alveolar socket treatment to
maintain natural architecture, platform switching, aesthetically appealing flap designs, innovative methods for closing soft tissues that offer
better visualization during second-stage surgery
with less scarring, inlay connective tissue grafts,
which make up a large portion of contemporary
implant therapy, and onlay grafting techniques
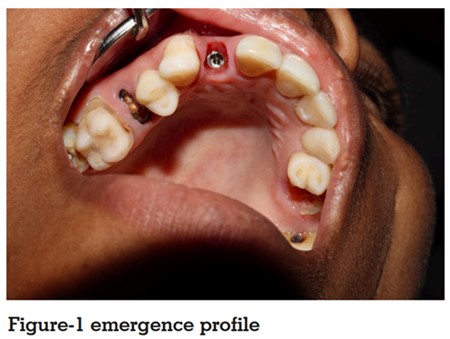
to expand the keratinized band zone or stop further soft tissue recession In the anterior region,
developing an emergence profile (figure -1) have
become more crucial to the success of implant
restorations because they aim to closely mimic
the natural teeth and produce an equilibrium between the blend of hard and soft tissue contours.
The development of the peri-implant zone which primarily comprises of the crestal bone and the surrounding healthy soft tissue are considered to be of paramount necessity for the long-term success of implant-supported restorations. Factors governing the peri-implant zone esthetics include the following:
The evaluation of the aesthetic success of the
peri-implant architecture is determined by the
white aesthetic score and pink aesthetic score.
Esthetic Criteria – Pink & White Score
Esthetic considerations of implant crowns on anterior teeth uses different proportions, including
“red” as well as golden proportions. The pink
aesthetic score was developed by Furhauser et
al7
. while the white aesthetic score was defined
by Belser et al8. (table-3) and they aid in assessing the soft tissue esthetics around implant
placement.
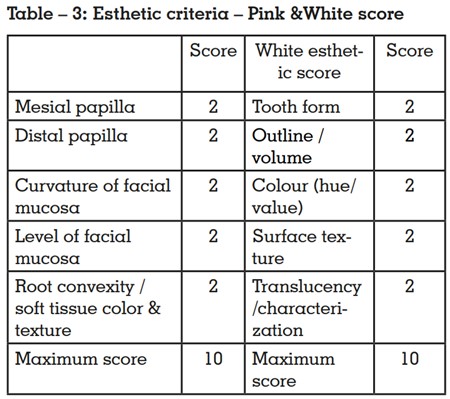
The Pink esthetic score is based on variables
such as mesial papilla, distal papilla, soft-tissue
level, soft tissue contour, alveolar process deficiency, soft-tissue color and texture. Each variable is assessed with a 2-1-0 score, with 2 being the best and 0 being the poorest score. The
highest possible score reflecting a perfect match
of the peri-implant soft tissue with that of the reference tooth.
Provisionalization
The provisional restoration is a critical component
of an overall treatment plan as it affords the opportunity to critically evaluate the function and aesthetics in a material which can be easily manipulated.
Provisionalisation in implant rehabilitation provides esthetics, maintains masticatory ability, and
preserves space as they intend to preserve and ultimately control the peri-implant hard and soft tissues by mastering the restorative material stacked
between the implant shoulder and that portion of
the restoration which is visible supra gingivally.
Fabrication and manipulation of the provisional
restoration give both the clinician and patient an
opportunity to slowly manipulate the peri-implant
tissues for the benefit of contours and ultimately the
aesthetic advantage. Once functional surfaces, restorative contours, tissue margins and dento-gingival complex profiles are established to both the patients and clinician’s approval, then they are able to
proceed with the definitive restoration9.
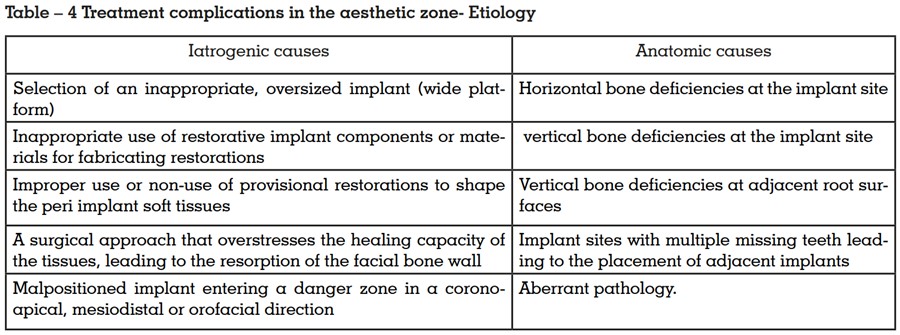
Treatment complications in the aesthetic zone
Esthetic failures are predominantly caused by inappropriate implant positioning and/or improper
implant selection10. Treatment complications can
range from fracture of the prosthetic components
to a transient inflammatory condition; however,
this article addresses the possible complications
in the esthetic zone (table-4), which involves the
possibility of failure only due to esthetic reasons.
Many esthetic complications can be prevented
if adequate presurgical planning is done, and
appropriate corrective measures taken during
surgical phase, and subsequently the prosthetic
phase.
The goal is to create gingiva and related structures that look beautiful and natural. Optimizing
techniques unique to the pre-prosthetic, pre-implant, and prosthetic stages is largely responsible
for maximising the esthetic outcome. Therefore,
given the dynamic stature of the modern implant
therapy, the art of incorporating a desirable
implant-supported prosthesis towards a beautiful
smile requires a thorough aesthetic diagnosis,
a holistic approach to implant construction, and
careful implementation of the planned treatment
from a contemporary perspective. Having reasonably contemplated the aesthetic principles of
importance in implant rehabilitation, the present
review attempts to cover an overall picture in attaining perfection in aesthetics especially red or
soft tissue aesthetics. Futuristic studies regarding
the aesthetic outcome can further be enhanced by
utilizing cutting-edge digital technologies involving software applications for evaluating clinical
and biological indicators of the prosthetic field of
view, virtual planning of implant positioning, and
design forecasting of future prosthesis.