

Aims: To analyze impact of different implant
placement timings on the esthetic stability of a single
implant restoration in maxillary anterior region.
Materials and methods: The systematic review and
meta-analysis adhered to the PRISMA guidelines
and were registered in the PROSPERO database.
In addition to systematic searches on the national
library of medicine (MEDLINE PubMed), Cochrane
library, Google Scholar, and EbscoHost, manual
searches were also conducted to identify articles
published from January 1, 2000, to December 1,
2020. The included studies comprised randomized
controlled trials, as well as prospective and
retrospective cohort clinical studies. The assessment
of risk of bias employed the Cochrane Collaboration’s
tool, MINORS tool, and a quality appraisal checklist.
Utilizing the Review Manager software tool, a metaanalysis was conducted, and the robustness of the
meta-analytic findings was duly evaluated.
Results: Out of 313 studies screened, seven met the predetermined inclusion and exclusion criteria for
incorporation into the systematic review. The metaanalysis disclosed an effect on marginal bone loss
associated with different implant placement timings.
However, the overall impact on esthetic stability was
not statistically significant. Furthermore, there is
moderate evidence suggesting a decrease in marginal
bone loss following immediate implant placement,
with a mean difference of -0.33mm.
Conclusions: The timing of implant placement appears
to have some impact on both marginal bone loss and
pink esthetic score. However, no statistically significant
difference was observed when comparing various
implant placement timings in terms of pink esthetic
score and marginal bone loss. The evidence lacked
sufficient strength to firmly support the aforementioned
observations, emphasizing the need for additional
well-designed randomized clinical trials to draw
definitive conclusions.
Key words: dental implants, single-tooth implants, marginal bone loss, pink esthetic score.
Rehabilitating the maxillary anterior region poses a formidable challenge due to the heightened
visibility and aesthetic expectations of patients.1
This complexity in dental implant restoration
arises from factors like reduced buccal bone volume, bone angulation, thin biotype, and a higher incidence of soft tissue defects.2
The esthetic outcome of implants is further influenced by
variables such as the patient’s smile line, tooth
and root positions, biotype of the periodontium,
tooth shape, bone anatomy of the implant site,
and optimal implant positioning.3
The timing of
implant placement is also considered a crucial
factor affecting esthetic outcomes.4
Various classifications for the timing of implant placement
after tooth extraction exist, with one of the earliest attempts in 1993 introducing terms like immediate, recent, delayed, and mature.5
The widely
accepted classification from the Third International Team for Implantology (ITI) consensus
conference categorizes implant placement into
types 1, 2, and 3.6 Type 1 (immediate implant
placement) involves placing implants in fresh
extraction sockets within 24 hours. Type 2 (early implant placement) sees implants positioned
approximately 4 to 8 weeks (up to 16 weeks) after tooth extraction. In Type 3 (late/conventional
implant placement), implants are placed once
most dimensional changes in the alveolar ridge
have occurred, typically after 16 weeks.
When rehabilitating the maxillary anterior region, esthetic outcome is of paramount importance.7-10 The primary determinants for evaluating esthetic stability are marginal bone and
soft tissues.10 Marginal bone level, measured
from the implant platform to the alveolar crest,
assesses hard tissue changes. For soft tissue esthetic evaluation, the commonly used aesthetic
index is the Pink Esthetic Score (PES).10,11 PES
incorporates variables such as soft tissue color,
soft tissue level, mesial and distal papilla, alveolar process deficiency, soft tissue contour, and soft tissue texture—critical factors in assessing
the overall health and aesthetics of the soft tissues surrounding the implant. These variables
are considered in peri-implant soft tissue evaluation to ensure not only the functional success of
the implant but also its aesthetic harmony with
the surrounding natural teeth and tissues.
Several studies and systematic reviews have
compared different implant placement timings
for single and multiple implant restorations
concerning esthetic stability.12-14 The majority of
these studies have included regenerative and
augmentation procedures in their assessment
of esthetic outcomes. However, few studies have
focused on evaluating the effect of different implant placement timings on esthetic outcomes
specifically in non-augmented sites. Therefore,
this systematic review aims to compare the effects of different implant placement timing protocols—immediate implant placement, early implant placement, or late implant placement—for
enhanced esthetic stability, considering parameters such as Pink Esthetic Score and marginal
bone loss.
Prospero registration and search protocol
In the course of this systematic review, the final
protocol was developed following an analysis of
findings from the initial pilot search. The protocol adheres to the PRISMA (Preferred Reporting
Items for Systematic Reviews and Meta-Analyses) guidelines. Following the formulation of
the protocol, it was registered on the PROSPERO website, and the corresponding registration
number for this study is CRD42020189405.
Focus question
The focused research question was as follows:
“Do the immediate implant placement (IIP) and
early implant placement (EIP) have same effect
on esthetic stability of single implant restoration
in maxillary anterior region as late implant placement?”
PICO
The PICO (patient, intervention, comparison
and outcome) formulated to answer the focused
question was
P: Studies with single implant restoration in
maxillary anterior region (premolar to premolar)
I 1: Immediate implant placement (IIP) placed
within 24hrs in fresh extraction socket
I 2: Early implant placement (EIP) with soft tissue
healing within 4-8 weeks or partial bone healing
within 12-16 weeks after extraction
C: Late implant placement (LIP) in healed bone
more than 16weeks after extraction.
O: Esthetic stability by means of pink aesthetic
score and marginal bone loss.
Inclusion Criteria:
Exclusion Criteria:
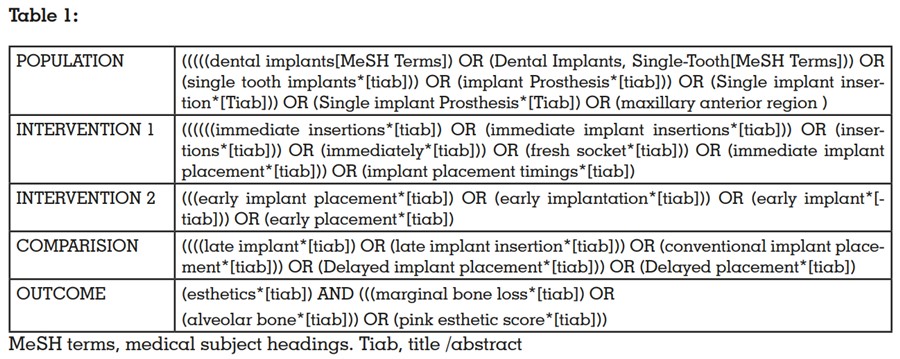
Systematic electronic searches encompassed
multiple databases, including the National Library of Medicine (MEDLINE PubMed), Cochrane
Library, Google Scholar, and EbscoHost-Dentistry. Additionally, manual searches were conducted in pertinent journals, and cross-referencing
of selected studies was meticulously performed
to identify additional articles meeting the eligibility criteria. To structure the search strategy, a
concept table was devised based on the PICO
criteria, incorporating key concepts, controlled
vocabulary terms, and free text terms. The acquisition of Medical Subject Headings (MeSH
Terms) involved querying key concepts within
the MeSH database, a controlled vocabulary
thesaurus employed by the National Library of
Medicine (NLM) for indexing articles in the MEDLINE PubMed database. (Table 1)
Two blinded independent reviewers, Y.S. and
G.A., independently performed this step, and in instances of disagreement, a third reviewer,
S.N., was consulted. Inter-examiner agreement
was assessed using the Kappa (K) test for each
reviewer’s searches. The data underwent statistical analysis utilizing the Statistical Package for
the Social Sciences (SPSS v 26.0, IBM). Statistical significance was determined at p < 0.05, with
an α error of 5% and a β error of 20%, ensuring
an 80% power for the study. The overall K value
was 0.97, and individual values for specific databases were as follows: National Library of Medicine (MEDLINE PubMed) (K = 0.901), EbscoHost-Dentistry (K = 1.000), Cochrane (K = 0.827),
and Google Scholar (K = 0.949), demonstrating
the agreement between reviewers’ searches.
Conflicts were resolved through discussion of
each article until consensus was reached. Efforts
were made to contact corresponding authors of
included studies for the retrieval of any missing
information or clarification of specific items.
Following the initial literature search, all articles
were screened to eliminate irrelevant publications, in vitro and animal studies, case reports,
case series, and review articles. Studies were
screened further based on relevance of data reported in abstracts. Finally, the full texts of the
selected papers were examined to confirm study
eligibility, following the inclusion and exclusion
criteria for included studies.
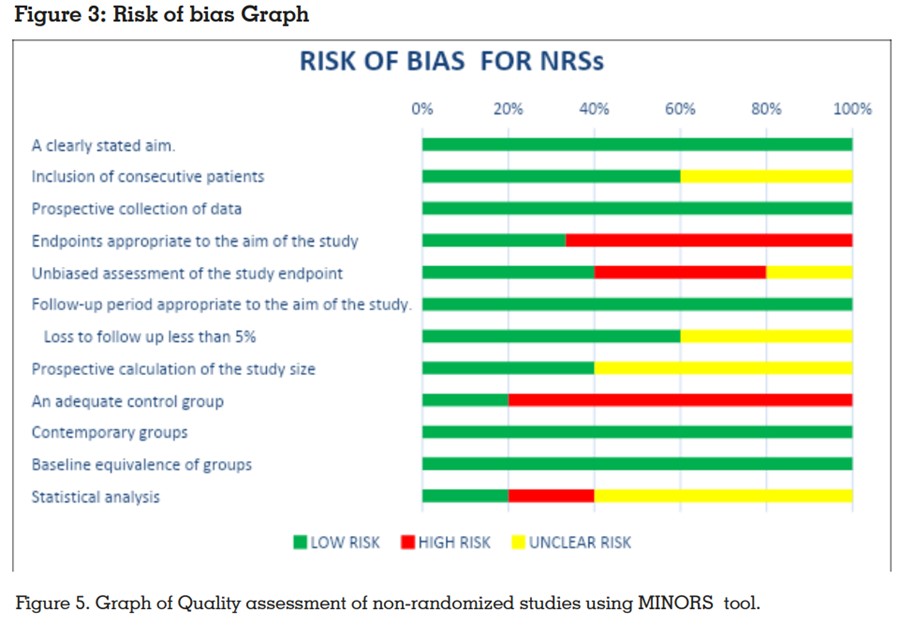
Two reviewers, namely Y.S. and G.A., independently evaluated the risk of bias. Quality
assessment for included randomized controlled
studies utilized the Cochrane Collaboration’s
tool (RevMan 5.4), evaluating seven criteria: random sequence generation (selection bias), allocation concealment (selection bias), blinding of
participants and personnel (performance bias),
blinding of outcome assessment (detection
bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other
bias. Studies were categorized as low risk if they
met all criteria, moderate risk if one criterion
was missed, and high risk if two or more were
missed. For five non-randomized studies, the MINORS (Methodological Items for Non-Randomized Studies) 16 scale was employed.
Statistical analysis
In terms of statistical analysis, the extracted data
underwent assessment using the Cochrane Collaboration’s tool, RevMan 5.4, to examine the relationship between esthetic stability and implant
placement timings. The analysis applied the
inverse variance method to continuous outcome
variables, presenting effect sizes as mean differences or standardized mean differences, along
with 95% confidence intervals (CI). Forest plots
were generated for both overall and subgroup
analyses to depict effect sizes. Additionally, a
funnel plot was created for the primary outcome
variable to evaluate potential publication bias
across studies. The significance level for the
analysis was pre-set at 0.05. Mean and standard
deviation values for immediate, early, and late
implant placement (with marginal bone loss and
pink esthetic score), along with the number of
specimens per group, were utilized to calculate
the mean difference with a 95% CI. A random-effect model was employed when studies were not
functionally equivalent for generalizing results
from the meta-analysis. Heterogeneity was assessed using the I2 index, considering values
close to 0% as indicative of non-heterogeneity,
close to 25% as low heterogeneity, close to 50%
as moderate heterogeneity, and close to 75% as
high heterogeneity between studies.
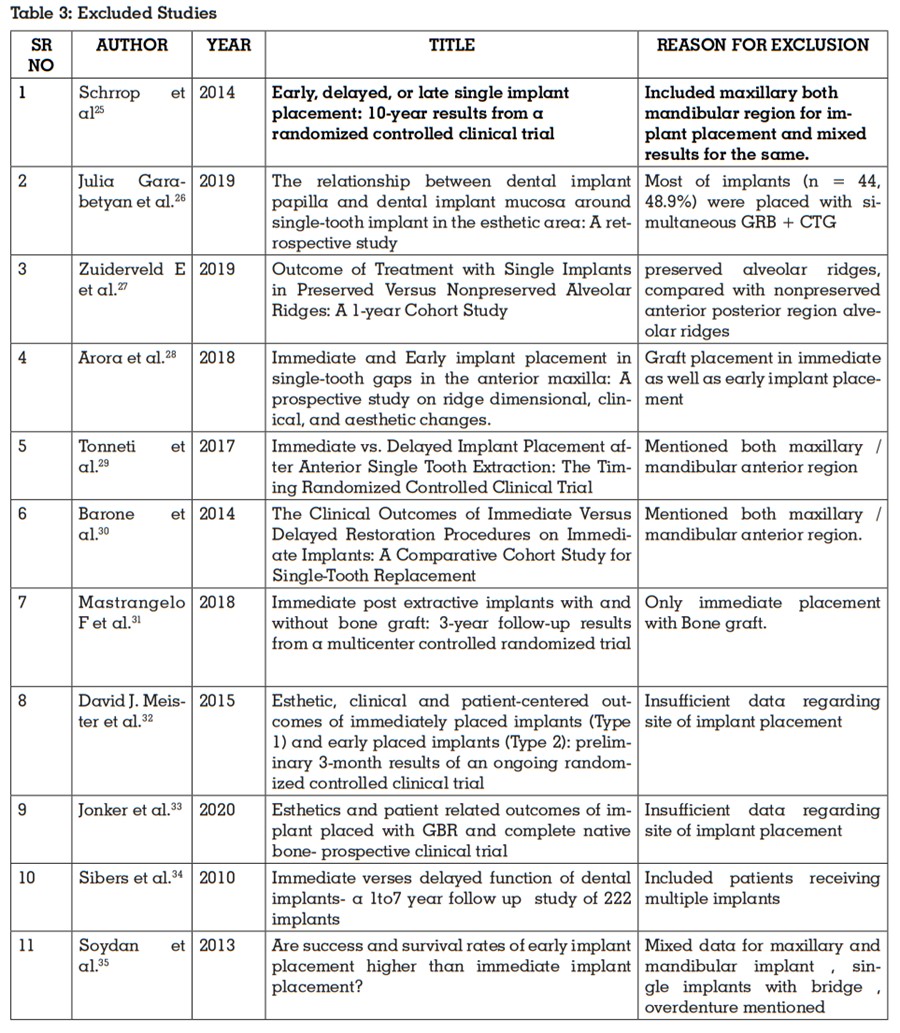
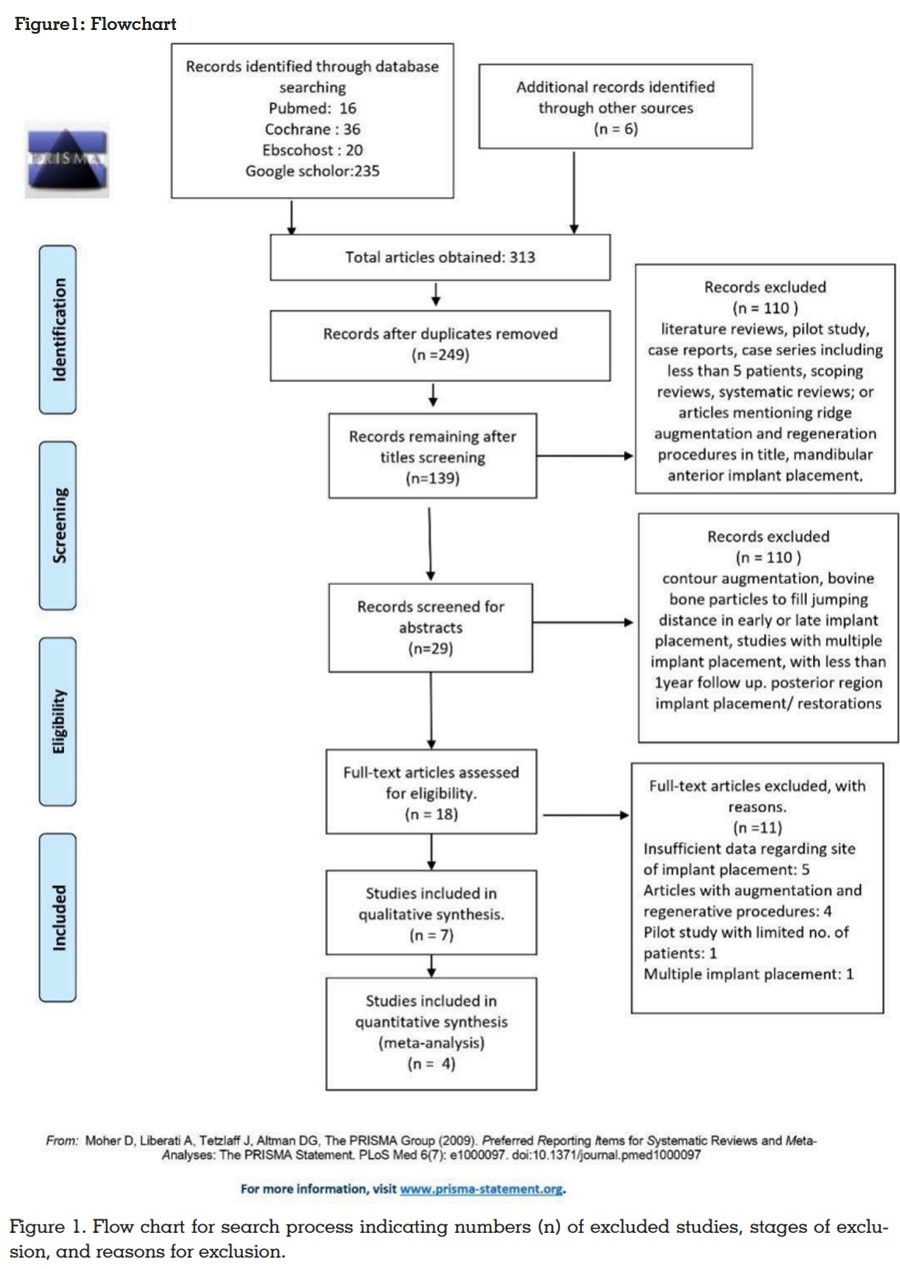
Description of studies
Total of 313 articles that were obtained through
the electronic searches were exported into the
Mendeley Desktop software. The six articles obtained through the manual search were added
to the software manually. Two hundred and forty-nine (249) articles were left after the elimination of duplicates and were subsequently taken
into further consideration for the data selection
process. Out of these, 110 articles were excluded after screening of the title. Twenty nine (29)
articles were left after abstract screening. Seven
articles met the inclusion and exclusion criteria
and were thus selected in this systematic review.
The findings of the comprehensive electronic
and manual searches are consolidated in Figure 1, following the PRISMA (preferred reporting
items for systematic reviews and meta-analyses)
flowchart. All included studies reported Ethics
Committee approval. Participant characteristics
among the selected studies are summarized in
Table 2. Clinical characteristics and outcomes
from the selected studies are summarized in Table 3.17-24 Two studies out of seven were randomized controlled studies and five were non-randomized controlled trials.
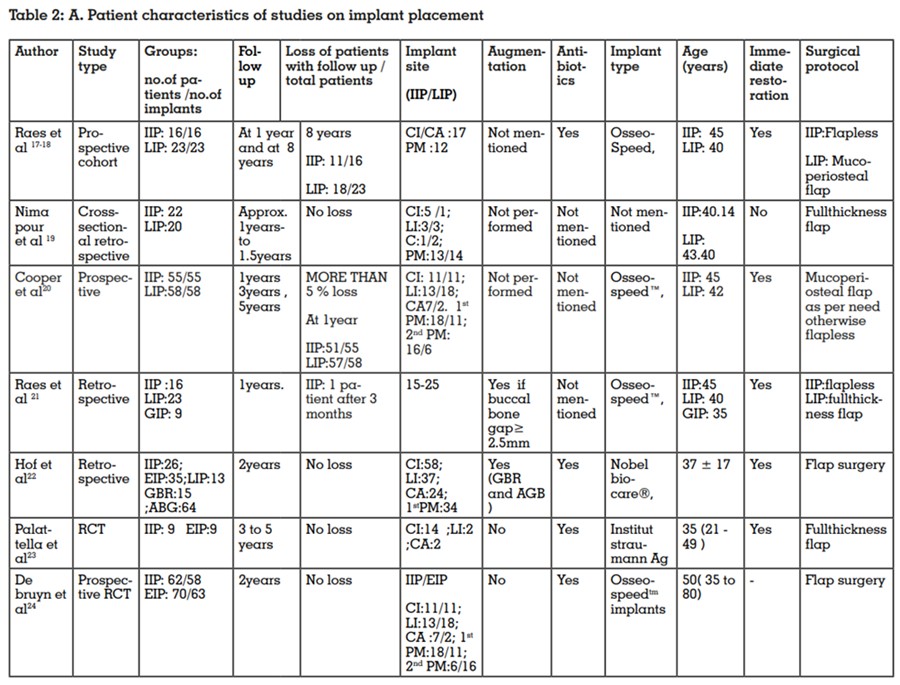
This systematic review is based on seven clinical
studies examining single implants with follow-up
periods ranging from 12 to 96 months. Out of 497
implants, data from 453 were available for evaluation, allowing a comparison of different implant placement timings. At the conclusion of the studies, 446 patients who had undergone a total
of 453 single implants (171 Immediate Implant
Placement (IIP), 49 Early Implant Placement
(EIP), and 187 Late Implant Placement (LIP))
were available for assessment, resulting in an
overall dropout rate of 9%. Notably, one study
reported selective loss of follow-up, with an 18%
dropout rate, specifically 31.3% following IIP
and 21.7% following LIP.18 More than 5 % loss
was observed in one study.20 Only one patient
loss with immediate placement was observed
in another similar study.21 Whereas no follow-up
loss was reported in studies with early implant
placement.22-24 The organized data for analysis
was categorized under distinct headers such as
Study ID, author and year of publication, study
type, groups, patients lost to follow-up, implant
site, hard tissue augmentation, antibiotics, implant type, age, restoration, surgical protocol.
The details are compiled in Table 1. Another
table for clinical outcomes was entered under
following headers: marginal bone level, buccal
bone thickness, pink esthetic score, patient’s satisfaction, vertical soft tissue level changes, pocket depth and other outcomes are noted in Table
2.
Postoperative antibiotics were administered in
most of the studies. 17-18,22-24 Cooper et al20 was not specific about use of antibiotics and Pour et al19
and Raes et al21 failed to mention about use of
antibiotics. Out of seven, six studies mentioned
about type of implant used with their brand name.
Astra Tech OsseoSpeed™ implants system was
used in four studies.17-18,20,21,24 Brånemark® MK-III
and Nobel Replace™Tapered, Nobel Bio care®,
Goteborg, Sweden was used in one study.22 and
TE Straumann G was used in study by Palattella et al23 and pour et al18 did not mention about
implant type. The common protocol across all studies incorporated implant placement along
with immediate provisional restoration, with
the final cementation performed 10 to 15 weeks
post-placement.
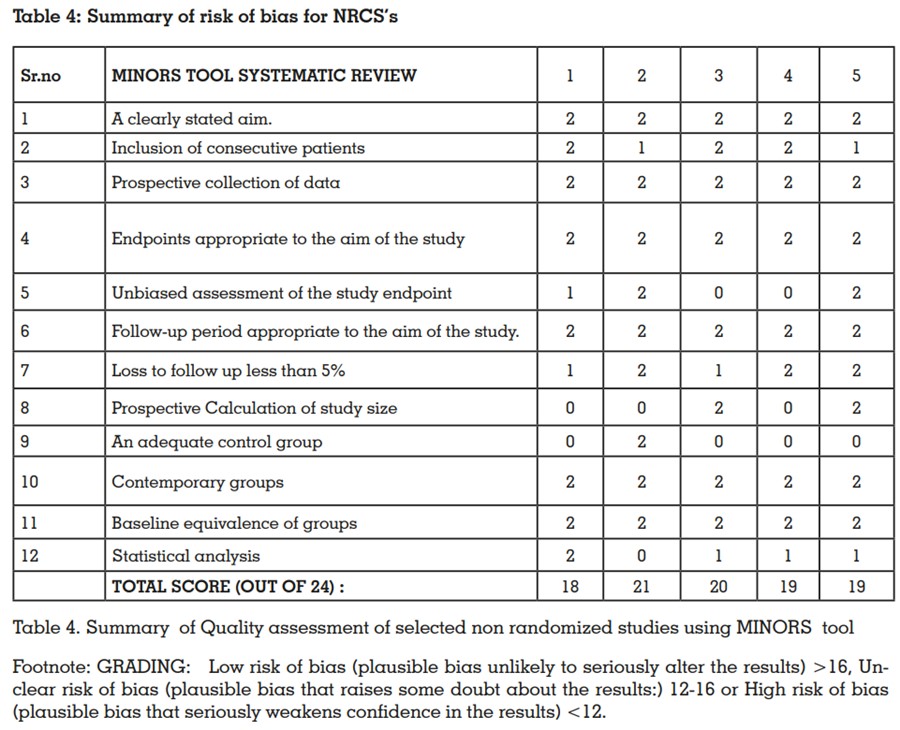
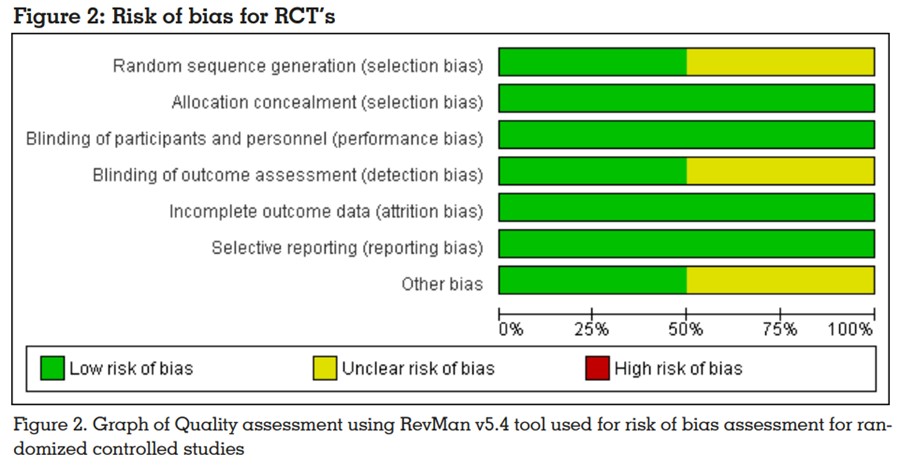
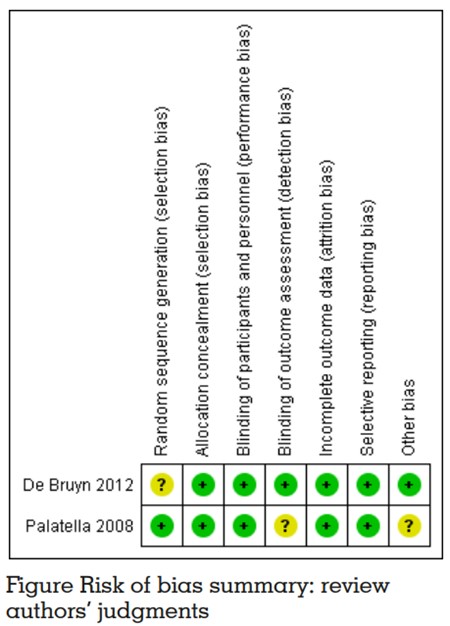
Risk of bias in the individual studies
Both the randomized controlled trials included in
this study had shown were assessed as being at
unclear risk of bias because each of these trials
was at unclear risk of bias in one or more domains. (Figure no. 2)23, 24 Quality assessment of
these studies revealed good overall quality, with no identified high risk of bias for any criteria. According to the risk of bias assessment conducted
using the RevMan v5.4 tool, six criteria were determined to have a low risk of bias. For non-randomized studies MINORS (methodological items
for non-randomized studies) 16 scale was used.
The individual summary of risk of bias for the 12
points was plotted in the risk of bias graph. Categorization of scores was done as follows: Scores
greater than 16 were labeled as Low risk of bias,
indicating plausible bias unlikely to seriously alter the results; scores between 12 and 16 were
categorized as Unclear risk of bias, suggesting plausible bias that raises some doubt about the
results; and scores less than 12 were considered
as High risk of bias, reflecting plausible bias that
seriously weakens confidence in the results. All
studies showed low risk of bias with high quality of data as all studies scored above 16. The
included studies which seemed to be relatively
homogenous in their study design and outcome
variables considered for a quantitative analysis
by means of a meta-analysis. 19,20,21-24
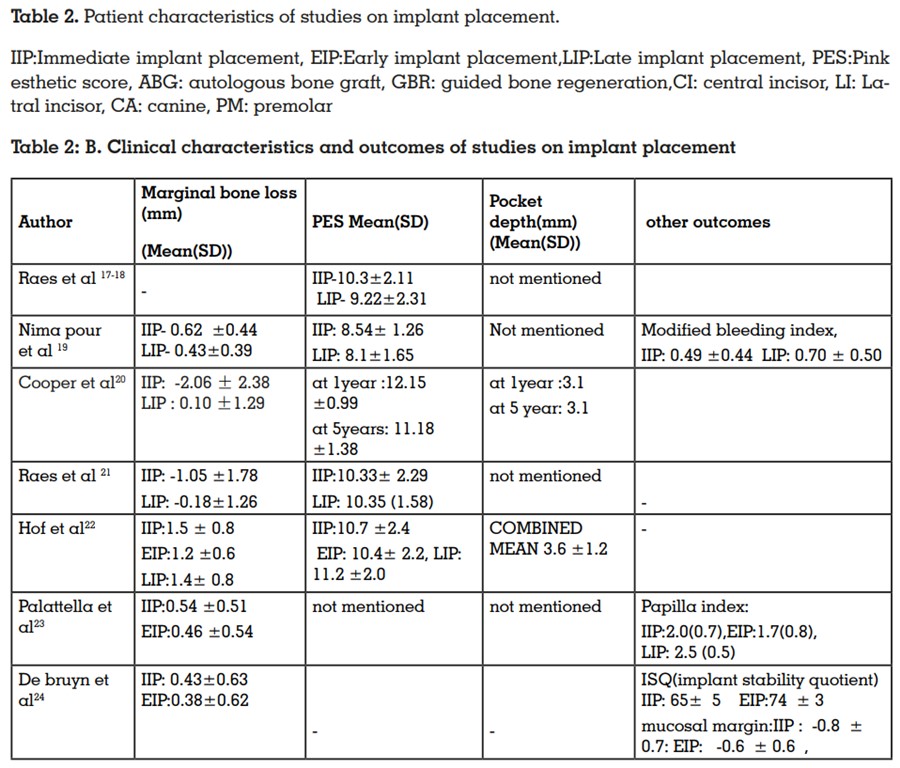
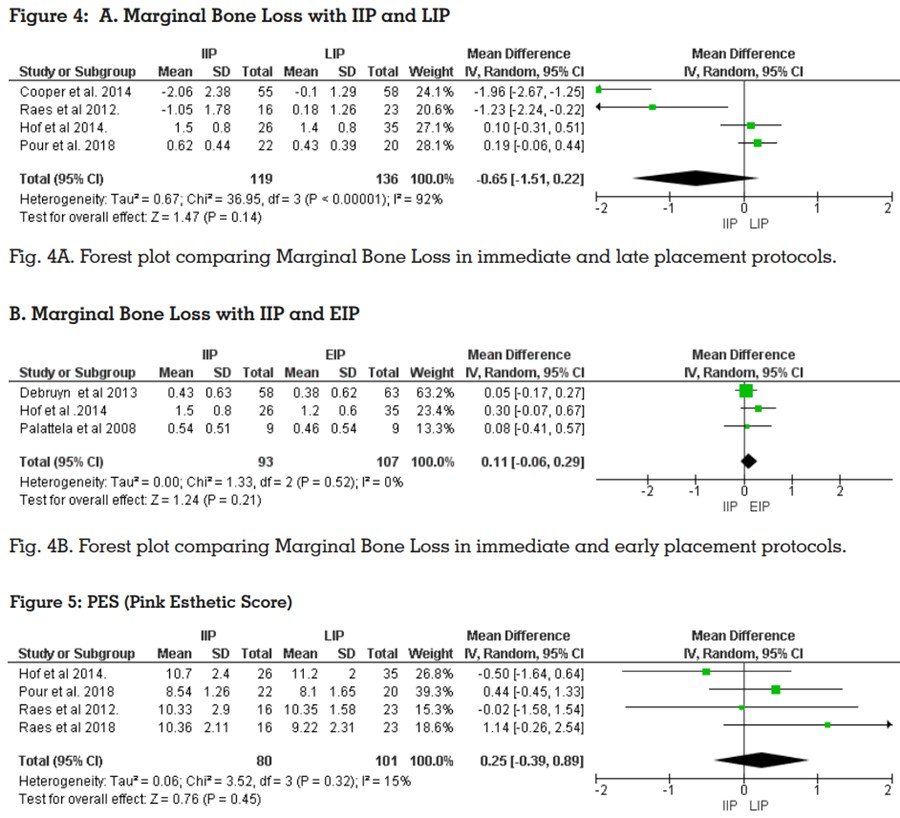
Primary outcome variable:
Marginal Bone Loss
Pour et al19, Cooper et al20, Raes et al21, Hof et al22 had discussed data on marginal bone levels with IIP and LIP. Cooper et al.20 showed significant bone gain in IIP and comparatively less
bone gain in LIP. De Bruyn et al24 and Palattella
et al 23 showed slight difference in bone levels in
IIP and EIP after implant placement.
Hof et al22 after comparing all three placement
timings (IIP,EIP,LIP), was found less bone loss
with EIP when compared to IIP and LIP. Meta-analysis on marginal bone loss showed no
significant difference comparing IIP and LIP and
IIP and EIP19,20,21-24 ( [ IIP Vs LIP (P = 0.14 , mean
difference = -0.65, 95% CI [-1.51 to 0.22]] and IIP
Vs EIP (P = 0.21, mean difference = 0.11, 95% CI
[-0.06, 0.29])) (Figure 4A and 4B)
Primary outcome variable:
Pink Esthetic Score
Four studies assessed the aesthetic outcome using the pink esthetic score (PES).17-18,.
19, 21, 22 Raes
et al.16-17, Raes et al.
21 and Hof et al.
22 utilized the
original PES index, resulting in a score based on
a total of 14 points. Pour et al.19 employed a modified PES index, generating a score on a total of
10.5 points.5 While Raes et al.17-18 and Pour et al. reported a slightly superior aesthetic outcome
for Immediate Implant Placement (IIP), whereas
Raes et al. 17-18 and Hof et al.22 described slightly higher pink esthetic scores for Late Implant
Placement (LIP).However, the meta-analysis did
not reveal a statistically significant difference
favoring one placement timing over the other (P
= 0.45, mean difference =0.25, 95% CI [-0.39 to
0.89]) (Figure 5)
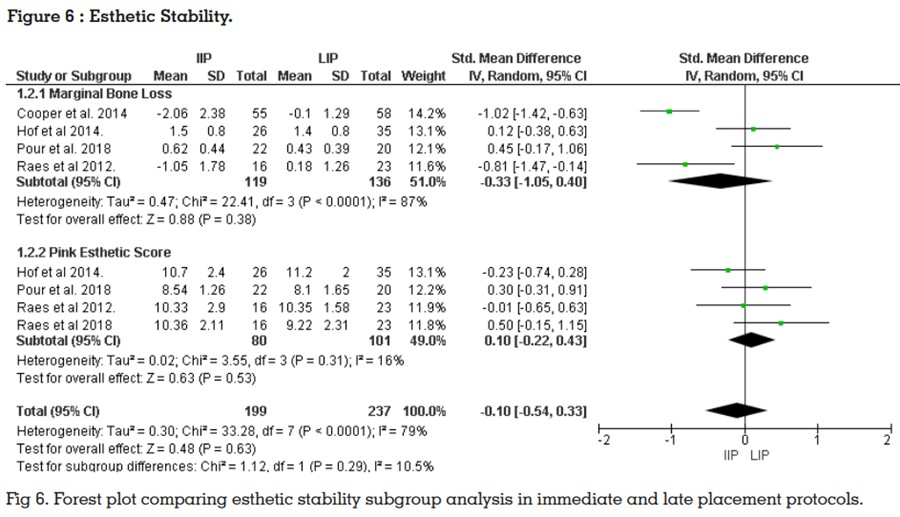
Esthetic stability:
Esthetic stability was evaluated in this study in
terms of Marginal Bone Loss and PES. A subgroup analysis was performed with all studies
included in meta-analysis with marginal bone
loss and pink esthetic score showed no significant difference for esthetic stability while comparing different implant placement timings. 17-24
(P = 0.29, SMD= -0.10, 95% CI (-0.54, 0.33)) (Figure 6)
Secondary outcome variables:
Buccal Bone Thickness:
Raes et al. 17-18 found that irrespective of timing
of placement, buccal bone wall less than 2 mm at 1-3-5 mm from the implant shoulder was observed at all implant sites with IIP and LIP with 8
years follow up. None of other studies evaluated
buccal bone thickness in anterior esthetic zone.
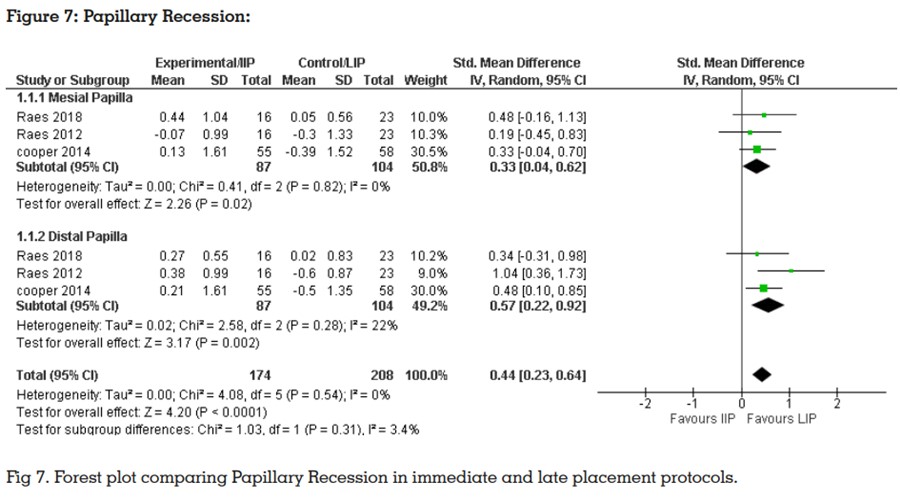
Papillary Recession (Figure 7)
Among the studies, Raes et al.17-18, Cooper et
al.
20 and Raes et al.21 were the only ones that detailed vertical changes in papilla height following Immediate Implant Placement (IIP) and Late
Implant Placement (LIP) and provided separate
data for the mesial and distal aspects. The overall analysis revealed statistically significant differences in papillary recession, indicating greater recession following LIP when compared to IIP
(Weighted Mean Difference [WMD] 0.44 mm,
95% CI [0.23, 0.64], P = 0.002). Notably, there
was low heterogeneity across studies, with an I2
of 0% (P = 0.54)
Patients Satisfaction
Three out of seven studies evaluated patient
related outcome at different timing of implant
placement. Two studies performed Visual analogues scales (VAS) for general satisfaction,
comfort, speech, aesthetics, functional outcome,
and cleanability. High scores were given for all
parameters indicative of high patient satisfaction. Following IIP, 95% patient satisfaction was
found and with other placement timing satisfaction was less.
Oral health impact profile (OHIP-14) scale used
by Raes et al.17-18 compared patient satisfaction
at one year and eight years. There was a slight
but significant difference between 1 year and
at least 8 years of follow-up in the late implant
placement. (P = 0.042). Where it seems, patient
satisfaction is better in case late implant placement and comparatively less satisfied in case of
immediate implant with long term follow up.
The present review exclusively analyzed the
studies which placed implants at different timings without augmentation with follow up of at
least 1 year in maxillary anterior esthetic zone.
While evaluating esthetic stability with the help
of hard and soft tissue levels by using some esthetic indices, meta-analysis suggested that immediate and late placement are equally beneficial for better success rate in clinical practice.
This systematic review could not suggest the superiority of any specific placement protocol over
the other for the marginal bone loss and pink
esthetic score.
In recent times there are many systematic reviews
related to anterior aesthetic zone to clarify what
is the best time to place the implant. Graziani
et al14 evaluated short- and long-term favorable
implant and patient related outcomes. But they
failed to establish whether early implant placement has different impact on bone regeneration
compared to late implant placement.14 Bassir et al.12 found that early placement has better stability over immediate placement in grafted and
non-grafted sites. But all these studies have assessed clinical performance only by measuring
implant survival and ignores peri‐implant conditions, like of soft and hard tissues, aesthetics
and patient related outcomes. These systematic reviews are inconclusive whether immediate
and early implant placement have similar effect
on esthetic stability as late implant placement.
Existing literature lacks systematic reviews that
assess esthetic stability in the maxillary anterior
region, particularly concerning factors such as
marginal bone loss and the Pink Esthetic Score
(PES). The importance of systematic reviews
in evaluating the health and esthetics of single-tooth dental implants cannot be overstated.
Consequently, this systematic review aims to investigate whether Immediate Implant Placement(IIP) or Early Implant Placement (EIP) is more
conducive to esthetic stability compared to Late
Implant Placement (LIP) in the anterior maxillary
region, with a focus on parameters like marginal
bone loss and the Pink Esthetic Score (PES)
The results of the present systematic review
support the hypothesis that immediate implant
placement (IIP) and early implant placement
(EIP) have same effect on esthetic stability of
single implant restoration in maxillary anterior
region as late implant placement since it has no
statistical significance.
With the help of a scoping review, it was observed that there are limited studies related to
different implant placement in non-augmented
or without any kind of tissue regeneration procedures in anterior esthetic zone immediate,
early and late with long term follow up. One of the most important key point of this systematic
review and meta-analysis was to focus on different implant placement timings in non-grafted
maxillary anterior esthetic zone, as critical analysis of this long‐term data can help identify and
improve current treatment strategies in implant
dentistry. At the same time many studies have
found that there is direct-indirect effect on marginal bone loss and pink esthetic score because of some factors like thickness of the buccal bone,
periodontal recession along with flap and flapless surgical procedures, timing of provisionalization, use of antibiotics, and restorations after
implant placement on anterior esthetic zone.35
Aesthetic outcome and buccal soft tissue height
of an implant-supported restoration would seem
to be indeed relevant. For aesthetic predictability of restoration, the thickness of the buccal bone
at the implant site played a fundamental role in
the rehabilitation.36,37 Hence, at the time of implant placement, this review focuses on the role
of the buccal bone thickness (BBT) on facial tissue stability. In present review, only one out of
seven studies, had discussed about thickness
of the buccal bone. Facial bone was missing in
the crestal area in 8 patients; late implant placement after long terms follow up of 8 years of
function (47%).17-18 Similarly, irrespective of timing of placement a buccal bone wall of less than
2 mm at 1-3-5 mm from the CEJ to implant was
observed at all tooth sites. To assess changes in
vertical soft tissue, two studies investigated implant placement combined with immediate restoration in the anterior segment of the dentition.
17-18,20 In these studies, the timing of provisionalization with the crown was established as the
baseline. However, Cooper et al20 suggested the
potential for papillary re-growth following Late
Implant Placement (LIP) due to the re-establishment of a contact point. Consequently, comparing Immediate Implant Placement (IIP) and LIP
in terms of papillary health may yield ambiguous results. Objective comparisons of papillary
and mid-facial recession can only be made between IIP and LIP when baseline registrations
occur with the original tooth still in place. Historically, there were no comparative studies examining such outcomes
In the present systematic review and meta-analysis, marginal bone loss did not show a significant difference between flap and flapless
procedures, regardless of what type of studies
were analyzed which is in line with the results
of earlier systematic reviews.34-36 This explained
that at the macroscopic scale the flapless procedure may not influence on bone remodeling.
Similarly, an analysis of three long term studies
with post-operative antibiotics demonstrated
similar trend for marginal bone loss towards IIP
site when compared with EIP22-24 (P = 0.21, mean
difference = 0.11, 95% CI [-0.06, 0.29]). These findings suggest use of antibiotics did not have
any significant effect on marginal bone loss with
long term clinical studies. Under subgroup analysis, the outcomes align with earlier findings,
indicating that the administration of post-operative antibiotics primarily contributes to the reduction of early implant loss following Immediate Implant Placement (IIP).39
The consideration of jumping distance is pivotal, particularly in cases of immediate implant
placement. Within this systematic review, bone
augmentation was undertaken at the time of implant placement in specific sites immediately after extraction, where a greater jumping distance
was observed. This approach was evident in
two out of seven studies, specifically in the investigations conducted by Raes et al. and Hof
et al.17,19 They observed early bone loss in these
augmented immediate placement sites whereas
bone gain in non-augmented immediate placement sites. In this review, the gingival response
after evaluation of anterior esthetic stability is
assessed by the Pink Esthetic Score (PES) from clinical photographs on the basis of six variables scored from 0→2. According to a systematic review by Graziani et al,14 it was not possible
to establish whether the early placement has a
different impact on bone regeneration. On further stratification of this outcome on the basis of
flap and flapless surgical procedures in esthetic
region, minor difference were revealed but for
safety issue flapless surgery has been preferred
as we have discussed earlier with respect to bone
loss. The analysis was performed with a limited
dataset, as Pink Esthetic Score (PES) data were
available from only four studies that reported on
anterior implants. The comparison specifically
concentrated on Immediate Implant Placement
(IIP) and Late Implant Placement (LIP), employing different scales for PES assessment.17-18,19,21,22
(P = 0.94, mean diff =0.02; 95% CI [-0.58 to 0.62
mm]).
While conducting this systematic review, notable
limitations emerged concerning both the quantity and quality of the available study material.
Of the two randomized controlled trials (RCTs)
incorporated, De Bruyn et al.24 and Palattella et
al.23 showed an unclear risk of bias, while the
remaining six nonrandomized studies demonstrated a low risk. The clarity of bias assessment becomes particularly crucial when making
comparisons of outcome variables among Immediate Implant Placement (IIP), Early Implant
Placement (EIP), and Late Implant Placement
(LIP). It is pertinent to mention that only one
study included in this review addressed a direct
comparison of all relevant parameters.22 In this
systematic review we had only two randomized
controlled trials out of seven which is very low for
any strong inference for direct comparisons of
different timing protocols.23,24 As it is not feasible
or ethical to perform randomized clinical studies to compare the different timings of implant
placement, we have included non-randomized
studies to provide evidence of the effect for interventions that are unlikely to be studied in randomized trials according to the recommendation
of the Cochrane handbook.15, 41 Hence, all study
designs with a control or comparison group were
considered for the inclusion in this study. Thus,
this systematic review could not suggest the precedence in any of implant placement timing protocol over the other for esthetic stability.
Based on results of this systematic review and meta-analysis, the following can be concluded:
Although no differences in soft tissue esthetic
outcomes were found between immediate, early
and late implant placement protocols, clinicians
should expect some soft tissue esthetic alterations after tooth extraction. Hence, this systematic review will help the clinician to decide the
best placement protocol considering the esthetic
stability using pink esthetic score and marginal
bone loss parameters in different clinical situations.
Conflict of interest statement: The author
reports no conflicts of interest related to this
study.
Source of funding: This study received no
external funding.