

Residual ridge resorption remains a significant concern in the field of prosthodontics and implant dentistry, posing challenges in the successful rehabilitation of edentulous patients. Residual ridge resorption is a common phenomenon following a tooth extraction, leading to significant changes in the alveolar ridge’s shape and volume. This review article aims to provide a comprehensive overview of the various treatment modalities available for managing residual ridge resorption. The case report presents a novel treatment modality for managing residual ridge resorption and its successful application in a clinical case.
Key words: Complete denture, Residual ridge resorption, all green technique, neutral zone, Management of residual ridge resorption, Denture stability
Bone, a living and mineralized tissue, experiences a perpetual cycle of resorption and regeneration throughout one’s lifetime. The structural and functional uniqueness of the bones in the
maxillofacial complex, including the jaw bones
and temporomandibular joints, stems from their
exposure to ongoing stresses during activities
like mastication. This process is known as bone
remodeling, which safeguards skeletal structural integrity while contributing metabolically to calcium and phosphorus balance. Old or
damaged bone is resorbed, making way for the
deposition of new bone material in a continual
process. Forces duration, magnitude, and application rate determine how bone integrity changes.[1] The residual ridge pertains to the segment
of the alveolar ridge and its overlaying soft tissue that persists subsequent to tooth extraction
or loss[2]. In 1971, Atwood characterized residual ridge resorption as a significant oral pathological condition[3]. The term “Residual Ridge
Resorption” denotes the progressive reduction
in size and configuration of the residual ridge
subsequent to tooth extraction. The success of
complete dentures hinges on fulfilling three fundamental properties: retention, stability, and
support. Mandibular dentures face greater challenges in achieving these due to the mandible
ridge’s reduced residual ridge for retention and
support, coupled with a faster resorption rate
compared to the maxilla. Research conducted
by Atwood and Tallgren suggests that mandibular bone resorption is four times greater than
that observed in the maxilla. Initial rapid reduction in residual ridge size occurs within the first
six months, followed by ongoing slower bone
resorption, resulting in substantial jaw structure
loss. This reduction significantly contributes to
instability and reduced retention, particularly
in mandibular complete dentures1
The inflammatory response is promptly initiated following
tooth extraction, leading to the temporary sealing of the extraction socket by a blood clot. The
structural alterations due to resorption-related
changes can be observed starting in the initial
week, concurrent with the proliferation of epithelial tissue. The residual alveolar ridge bone,
even post-wound healing, undergoes continual
catabolic remodeling throughout life. This constitutes a distinctive aspect of extraction wound
healing. Notably, residual ridge resorption is
most pronounced within the initial 3 to 6 months
post-extraction, subsequently diminishing gradually. Clinical observation readily captures instances of residual ridge resorption subsequent
to tooth extraction, though the precise sequence
of underlying biological events remains incompletely comprehended.
In the maxilla, the natural orientation of the teeth
generally points downward and outward. Consequently, bone reduction tends to occur in an
upward and inward direction. This resorption
process results in a reduction in the overall size
of the maxilla, impacting the denture-bearing
area or basal seat. The primary areas of bone
resorption in the maxilla are the occlusal, buccal, and labial surfaces. As a consequence, the
maxilla loses height, and the arch narrows from
side to side and becomes shorter from front to back. On the contrary, in the mandible, the anterior teeth tend to tilt upward and forward toward the occlusal plane, whereas the posterior
teeth are mostly vertical or have a slight lingual
inclination. Mandibular ridge resorption mainly
takes place from the occlusal surface. This resorption pattern tends to make the mandibular
arch appear wider, in contrast to the maxillary
arch, which becomes narrower. Residual ridge
resorption (RRR) manifests as a centripetal process in the maxilla, where bone reduction occurs
towards the center, leading to a decrease in arch
dimensions. In contrast, RRR exhibits a centrifugal pattern in the mandible, where resorption
primarily affects the outer areas of the ridge, resulting in a perceived widening of the arch.5
Preventive approach- In recognition of M.M. Devan’s work, it is essential to implement all required steps to enhance the outlook for the remaining natural teeth. Additionally, it is advisable to replace any missing teeth promptly as they are lost. There are several rehabilitation options available for individuals with partially edentulous conditions, including removable partial dentures (RPDs), complete partial dentures (CPDs), dental implants, tooth-supported overdentures, and precision attachments.[6] People with bone diseases should follow a diet that is high in proteins, vitamins, and minerals while reducing or eliminating their intake of refined carbohydrates, white flour, and white sugar. In crafting dietary recommendations, it’s important to consider the patient’s ability to chew and digest the prescribed foods.
Conventional approach- The conventional approach to rehabilitating resorbed residual ridge
includes the use of complete dentures, which
can be employed with or without prior surgical
intervention. Various impression techniques can
be employed to record the resorbed ridge.7
McCord and Tyson’s admixed technique8- A mixture of impression compound and green sticcompound, with a ratio of 3 parts impression
compound to 7 parts green stick compound by
weight, is immersed in a bowl of water heated
to 60°C. It is then kneaded together until it forms
a uniform mass that offers a working time of approximately 90 seconds. After removing the wax
spacer from the custom tray, this homogeneous
mass is loaded, and the patient is instructed to
perform various tongue movements.
All-green technique9- The green stick compound
is thoroughly kneaded until it achieves a uniform consistency. Subsequently, it is applied to
the special tray and border movements are executed. Finally, the ultimate impression is made
using zinc oxide eugenol.
Cocktail impression technique10- In this approach, a custom tray is meticulously created
using self-polymerizing acrylic resin, following the Dynamic Impression Technique. This
tray is designed with a 1 mm wax spacer and
cylindrical mandibular rests positioned in the
posterior region, raised to an increased vertical
height. The patient is instructed to close their
mouth so that these mandibular rest snugly fit
against the maxillary alveolar ridge. This fitting
helps stabilize the tray, preventing any unwanted forward-backward or side-to-side movement
during the definitive impression-taking process
The lingual surfaces of these mandibular rests
are deliberately crafted to be concave, providing ample space for the tongue to move freely
during functional activities. For the definitive impression, the McCord and Tyson technique designed for flat mandibular ridges is employed.
To record the functional state accurately, the patient is guided to perform specific actions such
as running their tongue along their lips, sucking
in their cheeks, pulling in their lips, and swallowing while keeping their mouth closed—similar to
the closed-mouth impression technique—until
the impression material solidifies.
Winkler Closed mouth functional impression
technique11- denture bases with occlusal rims are crafted on the primary cast. Jaw relation is
established to accurately capture the appropriate horizontal and vertical dimensions. To
enhance tissue compatibility, a conditioning
material is applied to the tissue surface of the
mandibular denture base. The patient is then instructed to close their mouth at the previously recorded vertical dimension and perform various
functional movements, including puffing, blowing, whistling, and smiling. This process involves
applying the tissue conditioner material three
times, with intervals of 8–10 minutes between
applications, during which the patient continues to make functional movements. Finally, the
definitive impression is taken using light body
addition silicone material, employing a closed mouth technique.
In 1931, Fish was the first to outline the impact
of polished surfaces on denture retention and
stability. He also introduced the concept of the
“neutral zone,” which is an area where forces in
the mouth are balanced for optimal denture fit
and function.12 The neutral zone is defined as the
potential space situated between the lips and
cheeks on one side and the tongue on the other.
It represents an area or position within the oral
cavity where the forces exerted by the tongue
and the cheeks or lips are in equilibrium. Two
clinical studies have highlighted the advantages of employing the neutral zone technique. In
one set of cinefluorographic studies13 conducted
by Sheppard, it was demonstrated that the muscles within the oral cavity help stabilize complete
dentures during functional use. In another clinical study led by Fahmy and Kharat14, patients’
chewing efficiency and satisfaction with complete dentures made using either conventional
or neutral zone techniques were evaluated. The
findings indicated that patients experienced
better chewing efficiency with conventional dentures. However, patients did not perceive any significant difference in masticatory performance
between conventionally fabricated dentures and
those created using the neutral zone technique. Notably, patients reported greater comfort and
improved speech clarity with dentures crafted
using the neutral zone approach compared to
their conventionally prepared dentures. These
studies suggest that the neutral zone strategy for
denture fabrication may offer benefits in specific
edentulous situations.
Teeth arrangement- Control of horizontal forces can be achieved through adjustments in
buccolingual cusp height, taking into account
the shape of the residual ridge and the available inter-arch space. Functional balance is attained by positioning teeth favourably relative to
the ridge crest. This approach ensures efficient
cutting and shearing during mastication and
allows for anterior tooth clearance to prevent
interference. The goal is to minimize occlusal
stop areas, thereby reducing pressure during
functional activities. To establish coordination
between the primary and secondary masticatory
organs, it is advisable to position teeth within the
neutral zone. Interestingly, non-anatomic teeth
have been associated with fewer denture sore
spots and less ridge resorption. Semi-anatomic
reverse curve posterior teeth are beneficial for
the lower ridge, while anatomic posterior teeth
tend to lead to increased denture soreness and
ridge resorption. Some studies suggest that anatomic posterior occlusion is preferable for lower
dentures, whereas non-anatomic posterior teeth
are better suited for upper dentures.1
Surgical intervention-encompasses a range of
preprosthetic procedures, including ridge augmentation, vestibuloplasty, distraction osteogenesis, shelf reconstruction, secondary epithelialization, and grafting techniques. While these
surgical methods can enhance denture prognosis, it’s important to note that they may not be
feasible in all cases. Factors like underlying
systemic health conditions or inadequate quality and quantity of available tissue may limit the
suitability of these procedures
Implant-Supported Prosthesis1: Advantages Offered by Implant-Supported Prostheses: i)
Preservation of Alveolar Bone: Implant-supported prostheses contribute to the maintenance of
alveolar bone structure. ii) Preservation of Occlusal Vertical Dimension: These prostheses help
retain the correct occlusal vertical dimension. iii)
Sustained Alveolar Bone Height: The height of
the alveolar bone remains stable as long as the
implants remain in a healthy condition. iv) Enhanced Psychological Well-Being: Patients often
experience improved psychological health and
confidence with implant-supported prostheses.
v) Restored Proprioception and Improved Bone
Quality: Implants can restore proprioception and
lead to increased trabeculation and bone density. vi) Enhanced Stability, Retention, and Speech:
Implant-supported prostheses offer superior stability, retention, and phonetic performance. vii)
Maintenance of Muscle Structure and Function:
These prostheses help in maintaining the structure and function of muscles involved in mastication and facial expression. The effectiveness of
prostheses supported by dental implants hinges
on the expertise and proficiency of the implant
specialist. It is closely linked to several factors,
including patient selection, choice of implant,
surgical approach, postoperative care, and the
patient’s satisfaction with the treatment.
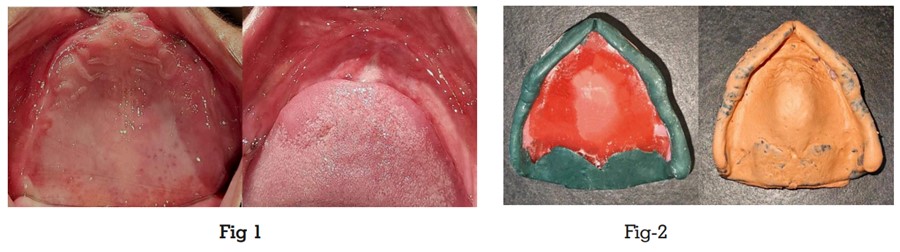
A 68-year-old female patient visited the Department of Prosthodontics at the Faculty of Dental
Sciences, SGT University in Haryana, India. She
had been edentulous for 8 years and complained
of loose mandibular dentures, which had been
causing discomfort and difficulty while eating
and speaking. She reported that this issue had
been progressively worsening over the past few
months. Upon intraoral examination, it was observed that the mandibular residual ridge had
undergone significant resorption, while the maxillary ridge had moderately resorbed (Fig 1). The
patient presented with compromised oral function and aesthetic concerns due to significant alveolar bone loss. medical history revealed
no significant systemic illnesses. Assessment of
oral hygiene was within acceptable limits and
there were no signs of oral lesions or pathologies. Considering the patient’s age and financial constraints, the patient was recommended
to undergo the fabrication of complete dentures
using the all-green technique and the neutral
zone technique.
Procedure-
Primary Impression- A preliminary
impressions were made of the maxillary and the
mandibular arches using an impression compound in a metal stock tray. The impressions
were thoroughly cleaned and subsequently
poured with impression plaster. Following this,
casts of maxilla and mandible were obtained,
onto which spacer wax was meticulously applied
and shaped.
Custom tray fabrication: A custom impression
tray was constructed using self-cure acrylic resin
(DPI-RR cold cure acrylic repair material) on the
primary cast. The tray’s border extension was
maintained at a distance of 2 mm from the vestibules.
Final impressions: For the maxillary arch, border moulding was carried out using green stick
i.e. low-fusing impression compound. This process aimed to replicate muscle activity, and record the functional depth and width of the sulcus.
Subsequently, the final impression was obtained
using a zinc oxide eugenol paste. (Fig 2). Due to
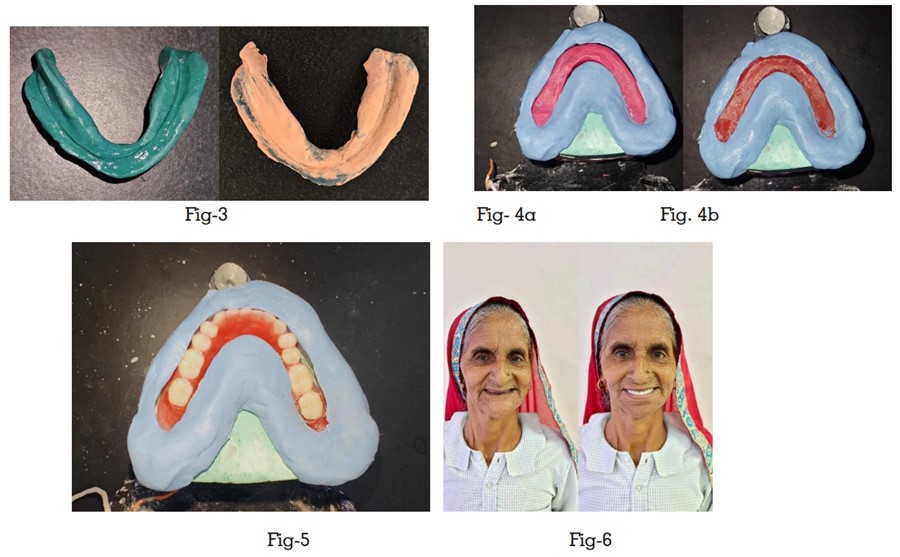
significant resorption of the mandibular alveolar ridge and a notably shallow sulcus depth, a secondary impression of the mandible was obtained using the “all green” technique. This involved kneading the green stick compound into
a uniform consistency, which was then loaded
onto the specialized tray, and the border movements were performed. Subsequently, the final
impression was made using zinc oxide eugenol
impression material (Fig 3).
Fabrication of base plate and wax occlusal
rims- The master cast was poured in dental
stone and the record base was constructed with
self-cure acrylic resin. The wax rims were fabricated and evaluated in terms of comfort, extension, and stability
Jaw relation: Traditional methods were employed to establish the jaw relation for capturing vertical and centric relationships, after which
the dental cast was mounted on the mean value
articulator. Subsequently, an additional pair of
record rims was constructed using new denture
bases replicated from the master cast. These
rims were made from impression compound
material. While keeping the maxillary rim in its
vertical position, the mandibular rim was adjusted to the same vertical height. Before recording
the neutral zone, the patient assumed a relaxed,
upright posture without any head support. Following this, the mandibular compound rim was
inserted into the patient’s mouth. A sequence of
activities mimicking physiological functions was
then guided, including smiling, grinning, pouting/pursing of lips, numerical counting, verbal
expression, pronouncing vowels, fluid intake, swallowing, gentle tongue protrusion, and lip
touching. This sequence was repeated over a
duration of 10 minutes until the compound became hard. Both compound rims were replaced
on the articulator to reassess the vertical relationship. A putty index was created surrounding
the molded impression compound rim (as shown
in Fig 4a). After removing the molded impression
compound rims from the base plate, the index
was placed in position. This index preserved
the dimensions of the neutral zone space. Then,
molten wax was carefully introduced into this
space, yielding a precise replica of the neutral
zone. The recently shaped wax rims were subsequently repositioned onto the articulator (Fig
4b). Accurate teeth arrangement was carried out
in direct accordance with the provided indices
(Fig 5). Throughout the teeth setup process, the
indices were employed to verify their placement
by aligning them around the wax try-in.
Try-in and insertion- Wax try-in of the denture was done. Then the dentures were processed,
finished, and polished in the conventional manner, and insertion was done (Fig 6).
The challenges associated with residual ridge resorption are numerous, with one of the most significant issues being the difficulty in retaining dentures. While osseointegrated dental implants have become the preferred option for complete rehabilitation, they also come with drawbacks such as high costs and surgical risks, especially when dealing with resorbed ridges that may require regenerative techniques. Additionally, medical and social factors, along with cost considerations, may make autogenous bone transplantation impractical for some patients. As a result, conventional dentures continue to be a viable solution for many aging individuals. The key to achieving proper denture retention, stability, and support lies in the impression of the completely edentulous arch. Various modifications to impression techniques have been attempted in the past to enhance these aspects.[15] The focus of this technique is on the primary impression, spacer design, secondary impression, and the choice of impression materials. Custom trays are employed to create ample room for the impression material, allowing for the capture of both the functional form of the primary stress-bearing region and the anatomical shape of the area that is not designed to endure functional loads. Greenstick compound is employed for border molding, a viscous material that molds tissues without compression. During the final impression, zinc oxide eugenol paste is used to accurately record the ridge with minimal pressure, capturing minute details of the residual ridge in its passive state. In the context of jaw relation, the neutral zone approach is employed to identify the neutral zone’s location, which helps determine the correct placement of teeth following ridge resorption. Many experts advocate for positioning the maxillary anterior teeth in proximity to the natural anterior teeth’s original location. Failure to do so could potentially lead to compromises in esthetics and speech for the patient. Moreover, the positioning of the maxillary teeth must align with the patient’s preferences. The neutral zone registration may indicate the need to reposition the mandibular anterior teeth slightly towards the lingual side. This adjustment can usually be performed without adversely affecting the denture’s aesthetic appeal. When the patient naturally molds their maxillary and mandibular ridges into the neutral zone during functional activities, the outcome is a denture that provides enhanced stability.[16]
The presented procedure outlines a straight forward, efficient, and dependable method for capturing impressions of a resorbed mandibular ridge. This technique involves the utilization of
a custom tray, green stick compound, and zinc
oxide eugenol impression material. Specifically, it focuses on imprinting the ridge’s crest in its
anatomical form and accurately records the primary stress-bearing area in its functional state,
promoting the long-term health of the surrounding tissues. This fusion of methods results in
prostheses with superior retention and stability.
By employing a viscous material within a closely
fitting tray, this technique allows for the physiological compression of tissues in the primary
stress-bearing areas, ensuring optimal adaptation and support. This technique offers an effective solution for clinicians dealing with patients
who have experienced mandibular ridge resorption. Its simplicity, speed, and focus on maintaining tissue health make it a promising addition to
the range of methods available for obtaining accurate impressions and ultimately contributing
to the success of prosthodontic treatments. The
neutral zone technique is considered one of the
most effective alternative approaches for dealing with severely atrophied mandibular residual
ridges.[17] However, it is infrequently employed
due to the additional clinical steps it entails and
its inherent complexity. Failures in both complete
and partial dentures can often be attributed to
not taking into account the considerations associated with the neutral zone.[18] Consequently, it
is crucial to assess the neutral zone as a critical
factor before making any alterations to the arch
form or the alignment of teeth.