

Abstract: Prosthodontic rehabilitation of patients undergoing ablative cancer procedures involves significant challenges and technicalities in the construction of a prosthesis like repeated prosthetic adjustments or remakes, and ultimately improving quality of life. Mandibular resection causes the mandible to deviate towards the defect, which causes loss of occlusion on the non-resected side, altered mandibular movements, cosmetic deformity, difficulty in swallowing, and impaired speech and articulation. Restoring speech, deglutition, mastication, and respiration in individuals who have undergone maxillary resection involving the maxillae, hard and soft palates, and paranasal sinuses is extremely difficult. It may not be feasible to surgically reconstruct in each case. In conjunction with physical therapy, prosthetic rehabilitation assists such patients in regaining form and function and improving their quality of life. It can be achieved by using obturators and mandibular guidance prosthesis, which could efficiently retrain the maxilla and mandible following surgical procedures to achieve a functional occlusal relation, enabling early progression leading to a permanent restoration that functions almost perfectly. This review’s objective is to highlight the various rehabilitative prosthesis that can be used to correct maxillary insufficiency and mandibular discontinuity defects following tumour resections using the available information.
Key words: rehabilitation, prosthesis, maxillofacial defects
The goal of oral rehabilitation in hemimandibulectomy patients is to prevent altered mandibular movements, disfigurement, swallowing
difficulty, impaired speech and articulation, and
mandibular deviation towards the resected site.
Various prosthetic options, such as maxillomandibular fixation, implant-supported prosthesis,
removable mandibular guide flange prosthesis, and palatal ramp restoration, can help achieve
this. A provisional appliance, such as a mandibular guide flange or palatal ramp prosthesis,
can be constructed to restore a normal maxilla-mandibular relationship.1
The maxillary sinus is the largest of the paranasal
sinuses and has the highest incidence of malignant sinus tumours. 20% of paranasal sinus cancers are in the ethmoid sinus, 80% in the antrum,
and less than 1% in the sphenoid and frontal sinus.2
One of the most difficult aspects of oral and
maxillofacial reconstruction is the reconstruction
of maxillary bone defects caused by pathological or congenital causes. The primary goal of
these reconstructive efforts is to protect and improve the patient’s quality of life by attempting
to restore the patient’s lost form and function.3
Maxillary neoplasms are commonly treated by
surgical resection of the maxilla and adjoining
structures (maxillectomy). The surgery often results in abnormal communication between the
oral and nasal cavities. The functional and aesthetic rehabilitation of these resected maxillary
deformities is a complicated task. The midfacial region is dominated by the maxillae, which
also contribute to important midfacial structures
such as the orbit, zygomaticomaxillary complex,
nasal unit, and stomatognathic complex.4 Prosthetic obturation’s main objectives include separating the oral cavity from the sinonasal cavities and closing the maxillectomy defects to prevent
regurgitation.5
Prosthetic measures at differing
stages assist patients in regaining aesthetic and
functional abilities. An effective obturator prosthesis enhances speech, mastication, swallowing, and aesthetics.6
Tumors may arise in the alveolar mucosa, in the
periosteum and bone of the mandible, or from
the dental elements requiring segmental or radical resection of the mandible. Squamous cell
carcinoma of the alveolar mucosa, ameloblastoma, and osseous sarcomas are prevalent among
these lesions.
Ameloblastoma is a rare odontogenic tumor
that tends to be locally invasive. It occurs in the
mandible 4 times more frequently than in the
maxilla. Although midline lesions have been described, ameloblastoma of the mandible often
appears as an indolent mass in the third molar
area. It is most prevalent during the 3rd and 4th
decades of life. Males and females are approximately equally affected.
About 10% of all oral cancers are Squamous cell
carcinomas of the gingiva and alveolar mucosa.
These carcinomas occur more frequently in the
mandible and the molar region is primarily affected. They occur more commonly in men than
in females (4:1). A 25.9% prevalence of HPV-associated head and neck squamous cell carcinoma
(HNSCC) was concluded through a systematic
review. In comparison to oral (23.5%) and laryngeal (24.0%) SCC, the prevalence of oropharyngeal squamous cell carcinoma (OPSCC) was
higher (35.6%).9
The majority of these tumours
develop in edentulous regions. Tumors often
spread to the floor of the mouth and the buccal
mucosa. Approximately 30% of patients initially
have regional metastasis, which first affects the
submandibular nodes. Squamous cell carcinoma of the mandibular alveolar ridge is primarily
treated surgically, with a marginal mandibular
resection in early lesions and a segmental resection in advanced lesions with extensive bony involvement. Squamous cell carcinoma of the
mandibular alveolar ridge is primarily treated
surgically, with a marginal mandibular resection
in early lesions and a segmental resection in advanced lesions with extensive bony involvement.
The remaining mandibular segment deviates toward the defect after a segmental or hemi mandibulectomy for squamous cell carcinoma, and
the mandibular occlusal plane rotates inferiorly.
Due to the loss of the tissue which controls the
mandibular movements, the deviation occurs.10
Osteosarcoma is the most frequent primary osseous malignancy, which involves the mandible
or maxilla 6 to 7% of the time. The most common
sites of involvement in the mandible are the premolar and molar regions, followed by the symphysis, angle, and ramus. A diffuse swelling or a
palpable, occasionally painful mass is the most
typical sign of osteosarcoma of the mandible. Involvement of the inferior alveolar nerve frequently causes paresthesia of the chin or lip. It typically takes 3 to 4 months for symptoms to manifest
before a diagnosis is made. Osteosarcoma presents as a destructive, ill-defined intraosseous lesion with or without an adjacent soft tissue mass
on radiographic examination.
In hemimandibulectomy, the mandible deviates
due to its loss of continuity, which further results
in aberrant muscle function and facial asymmetry resulting in aesthetic deformities, functional
impairment, and psychological consequences.9
At the vertical dimension of rest, the residual
mandibular segment retrudes and deviates towards the surgical side in patients who have had
a mandibular resection.
Mandibular guidance prosthesis
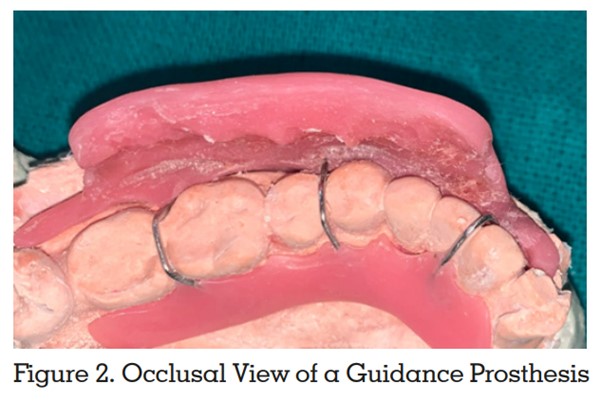
A palatal- or mandibular-based guiding prosthesis can be used for prosthetic rehabilitation
to achieve adequate occlusal function in such
patients.10 A mandibular removable partial denture is affixed to the guide flange on the non-resected side of a mandibular guiding prosthesis
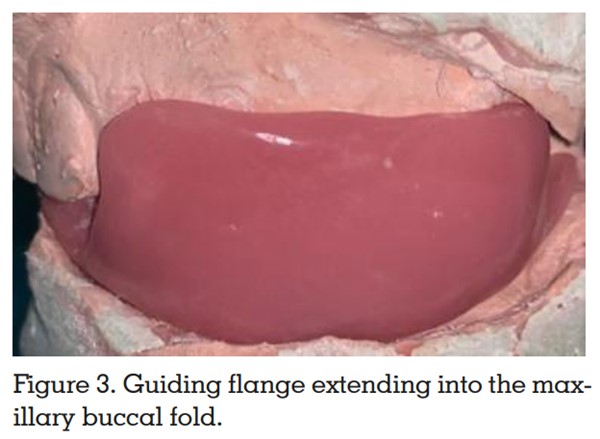
as shown in (Figure 2). By extending the flange
into the maxillary buccal fold, the remaining
mandibular segment is guided superiorly and
laterally to the desired jaw relationship which
can be seen in (Figure 3).11 “The flange mechanically holds the remaining mandible with
minimal to no lateral movement in the proper
position for the vertical chewing stroke.”12-14 This
extension can be made of acrylic resin, cast in
RPD metal, or wrapped in a thick wire loop.13–19
Although acrylic flanges can be adjusted in the
mouth, they are not rigid and are prone to abrasion, so they need to be reinforced with metal or
additional thickness. Metal flanges can be thin
and rigid, causing no distortion or abrasion of
the cheek space. For metal, however, the angle
and length must be predicted prior to casting because metal cannot be adjusted once it is inside
the patient’s mouth. The flange should be “extended 7 to 10 mm from the mandibular RPD in a
superior and diagonal position, shorter than the
maxillary vestibular depth.”12-14 More specialized techniques for determining the flange angulation are now required due to individual variations in the maxillo-mandibular relationship,
mandibular deviation in terms of degree, muscle
potency, and the ability to orient the lower jaw towards the non-resected side. Various guidance
prosthesis can be used to accomplish this. Mandibular guidance prostheses are broadly classified into two types:
Maxillary inclined plane prosthesis
On the non-defect side, palatal to the maxillary
teeth, a functionally generated occlusal record is
used and an occlusal table is fabricated which
slopes away from the natural teeth occlusally.
Interproximal ball clasps or Adams clasps are
used to retain the prosthesis. Due to the residual mandible’s medial deviation, mandibular
closure causes the remaining mandibular teeth
to gradually slide up the incline in a superior
and lateral position until the occlusal contact is
made. The extent of the deviation determines the
duration of wear. Positioning prosthesis with palatal flange can be used in patients who can use
their pre-surgical intercuspal position after mandibular resection with complaints of inability to
prevent the mandible from deviating towards
the defect side during sleep. They struggle to
reestablish their normal occlusal contact after
waking up. Additionally, TMJ discomfort and
muscular ache are frequent problems. To reduce the nocturnal deviation, a palatal flange can be
extended inferiorly into the lingual vestibule between the lateral border of the tongue and the
lingual surface of the remaining mandible. This
flange can be constructed using auto-polymerizing acrylic resin. The palatal extension should
be adequate even when the mouth is open to
prevent medial deviation of the unresected jaw.
The flange shouldn’t impinge on the mandibular
lingual mucosa and should only make contact
with the lingual surfaces of the teeth when the
jaw is opening and closing.20
Intermaxillary fixation
For five to seven weeks, Aramany and Myers
recommended using intermaxillary fixation with
arch bars and elastics following surgical resection. The remaining mandible is retained in its
ideal maxillomandibular position, enabling scar
formation while the defect heals and the teeth
are in occlusion. In the immediate postoperative period, little to no muscle retraining may be
necessary with the use of intermaxillary fixation.
The amount of deviation appears to be inversely
related to how long the mandible is fixated.21, 22
Vacuum-formed PVC splints
This framework comprises upper and lower
splints which are fabricated using upper and
lower plaster models. The upper splint encompasses the palatal vault and all standing teeth
to provide the greatest amount of lateral stability. The vestibular flanges and teeth, which will
serve as the mandible’s closure guiding planes,
should be included in the lower splint. At the
intercuspal position, both the upper and lower
models are articulated. Both upper and lower
splints are then incorporated into the arches
and joined together by adding another layer of
heated polymer between them. Flanges and indentations on the lower part of the splint make
it simple to place the mandible and lower teeth
in the right occlusal relationship when the jaws
are closed. Since it is comfortable for the patient
to wear, the plastic splint effectively controls and gently restrains jaw motions. The patient may
also wear the apartment at night. Once the patient has been accustomed to the path of closure,
this appliance must be replaced by a more definite acrylic or metal appliance.15
Exercise program
To retrain the residual muscles, enhance the
maxillo-mandibular relation, minimize scar contracture, and reduce trismus, prosthetic treatment should be accompanied by a planned exercise program.23
Two weeks following surgery, the exercise regimen can commence. Simple mandibular opening and closing with and without the appliance
are performed, as well as the patient grabbing
the chin and repositioning the mandible away
from the surgery site.24
Maxillary obturators
Maxilla is the site of the majority of intraoral abnormalities, in the form of an opening into the
antrum and nasopharynx. The hard and soft
palates, alveolar ridges, and floor of the nasal
cavity may all be involved, or the opening may
be extremely small. Postoperative maxillary abnormalities predispose the patient to hypernasal
speech, nasal cavity fluid leakage, and compromised masticatory function.25
A maxillary obturator is used to repair the intraoral defects. In cases of partial or complete
maxillectomy, an obturator (Latin: obturare, to
stop up) is fabricated.25 Prosthetic rehabilitation
goals for total and partial maxillectomy patients
include separation of the oral and nasal cavities to allow adequate deglutition and articulation, possible support of the orbital contents to
prevent enophthalmos and diplopia, soft tissue
support to restore the midfacial contour, and an
acceptable aesthetic result.26 The following are
the indications for using an obturator::
A typical maxillectomy resection removes the
teeth and alveolar bone along the midline. Desjardins advocated for maintaining the alveolar
bone around teeth that were proximal to the defect.28
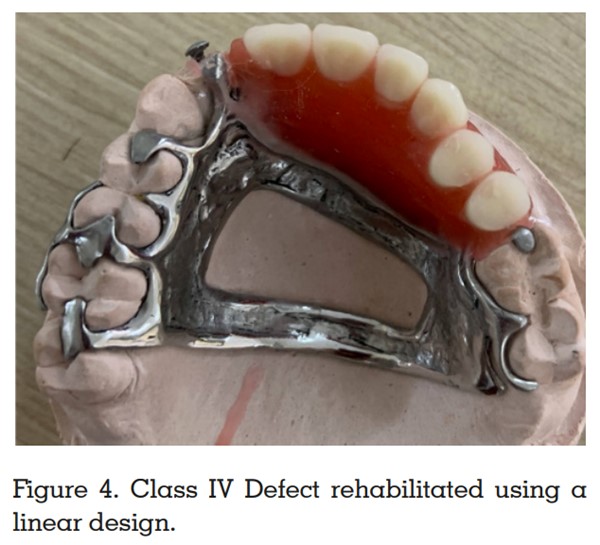
Either linear or tripodal design can be fabricated. Support is attained from the central incisor
and the most posterior abutment tooth while two
or three anterior teeth can be splinted, if possible. By placing a rest on the canine or the first
premolar’s distal surface in a tripodal configuration, the notion of efficient indirect retention is
applied when the dental arch is curved. Either
an I-bar on the central incisor or the labial surface of the anterior teeth with a gate design enables direct retention. The buccal surface of the
molars is used for posterior retention, while the
bracing is situated palatally. If the anterior teeth
are not incorporated into the design, a linear design is indicated.2
The premaxilla on the side with the defect is preserved. The bilateral design resembles a Kennedy Class II removable partial denture. In this
case, the tripodal design is indicated. It is advised to splint the two teeth located proximall the defect. The tooth closest to the defect and the
most posterior molar on the opposing side are
used for the primary support. The fulcrum line
and an indirect retainer are positioned as perpendicularly as possible. On the distal surfaces of the molar and the anterior tooth, guiding
planes are situated proximally. On all abutment
teeth, the buccal surfaces serve as the site for
retention, and the palatal surfaces serve as the
location for stabilizing components.29
The entire dentition is preserved, and the defect
is located in the center of the palate. It is constructed using a quadrilateral design. Premolars
and molars are used to provide support. The
buccal surfaces provide retention, while the palatal surfaces provide stability.29
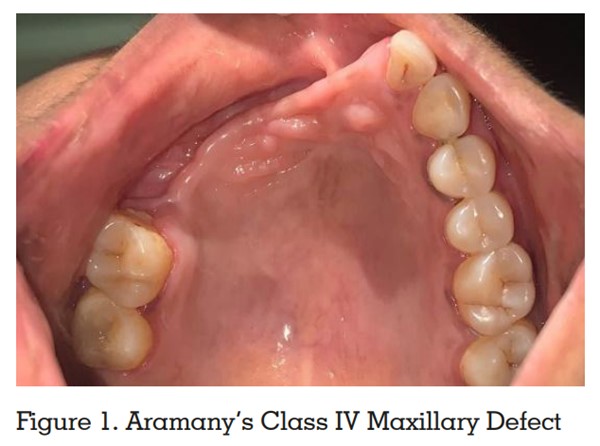
On the nonsurgerized side, the defect encompasses the premaxilla. A Linear design is recommended. All remaining teeth have support in the
middle, as seen in (Figure 4). On the premolars
and molars, respectively, retention is seen mesially and palatally. On the palatal surface of the
premolars and the buccal surface of the molars,
stabilizing components are attached.29
The hard palate, portions of the soft palate, and
the posterior teeth are resected while the anterior teeth are preserved. Two terminal abutment
teeth are advised to splint on each side. The
palatal surface of the most distal teeth provides
stability and support, while I-bar clasps are positioned bilaterally on their buccal surfaces. This
arrangement is basically tripodal. A gate prosthesis could also be fabricated in such cases as
an alternative.29
The least common class of anterior palatal defects is generally caused by trauma rather than
surgery. Such defects involve the bilateral splinting of two anterior teeth and they are joined together by a transverse splint bar. A quadrilateral
design is fabricated in case of a large defect or
when the remaining teeth have a poor prognosis.29
Due to the patient’s advanced age and the severity of the defect, rehabilitation for these patients continues to be an enormous challenge.
Numerous challenges associated with surgery
and prosthetic rehabilitation like lack of maxillary bone including pterygoid plates sometimes
zygomatic bone involvement, loss of lip support,
adherence of nasal and sinus mucosa with palatal mucosa, fibrosed palatal mucosa, lack of vertical guidance, reduced stress-bearing area, and
over closure of mandible need to be addressed.
Establishing normal function with low morbidity
and long-term sustainability must be the main
objective of these patients’ rehabilitation.30 Autografts are considered to be the gold standard
for management for these type of defects.31 But
there are associated problems with its use such
as selecting a suitable donor site, the morbidity of the donor site, especially for larger defects,
complications associated with tissue harvesting,
the discomfort of the patient, potential for infection both at the recipient’s and donor’s sites, the
additional skilled surgical team required, prolonged surgical time, and graft resorption. Due
to these restrictions, research is still being done
to find an appropriate alloplastic material and
accurate presurgical planning is needed to enhance craniofacial reconstruction.32
For mandibular defects, locking reconstruction
plates are advised to be used; however, these
plates must be properly bent to achieve the proper
mandibular contour. Preoperative plate bending
using three-dimensional (3D) stereolithographic models is becoming more and more popular
among surgeons.33 Engineering patient-specific
designs whose performance can be accurately
and precisely predicted will assist surgeons in
their routine procedures. The ability to precisely plan preoperatively, carry out virtual osteotomies or resections, and design patient-specific
implants are all facilitated by computer-assisted designing and manufacturing systems. Because of this cutting-edge technology, it is now
possible to create patient-specific implants using virtual designs and models.34 The advent of
computer-assisted design and manufacturing
techniques for maxillofacial reconstruction has
significantly improved surgical success since the
length and form of the implant may be customized to the needs of the patient and the surgeon’s
preferences.32, 35
Taking the entire stomatognathic system into
overview in both mandibular guidance therapy
as well as maxillectomy/midfacial defects classified as per the extent of resection, requires a
multidisciplinary approach viz. prosthetic (guidance prosthesis, inclined plane prosthesis), via
splints, IMF, grafts, obturators, etc. To provide the best treatment, one must employ a philosophic approach that would concentrate on selecting the most suitable material and technique
along with a good physiotherapy regimen for an
overall successful and positive rehabilitation experience.