

The implant abutment is a component that is still facing criticism in selection and usage due to the wide variety being made available in the market which puts the clinician in a dilemma to select the right choice. This article highlights the types, classification and important criteria which help in implant abutment selection and gives a brief review on the recent advances in implant abutments.
Key words: implant abutment, abutment selection, abutment material, abutment
Today, with the ever-increasing popularity on
dental implants, there are a wide variety of implant components and parts available. One of
the most confusticate tasks faced by an implant
clinician is the implant abutment selection.
Abutment selection during treatment planning
saves a lot of time and cost as it enables the clinician to decide for a stock or custom abutment
prior to surgery.
This article highlights the types, classification
and important criteria which help in implant
abutment selection and gives a brief review on
the recent advances in implant abutments.
There are 2 main systems integrating implant
components, the three-tier or two-tier system.
A three-tier system has three separate components, the implant, the abutment and the
crown whereas a two-tier system incorporates
two separate components, the abutment and the
crown to form a single unit and the implant is
a separate component or, the implant and the
abutment form a single unit and the crown is
separate.1
There are several classifications for implant abutments -
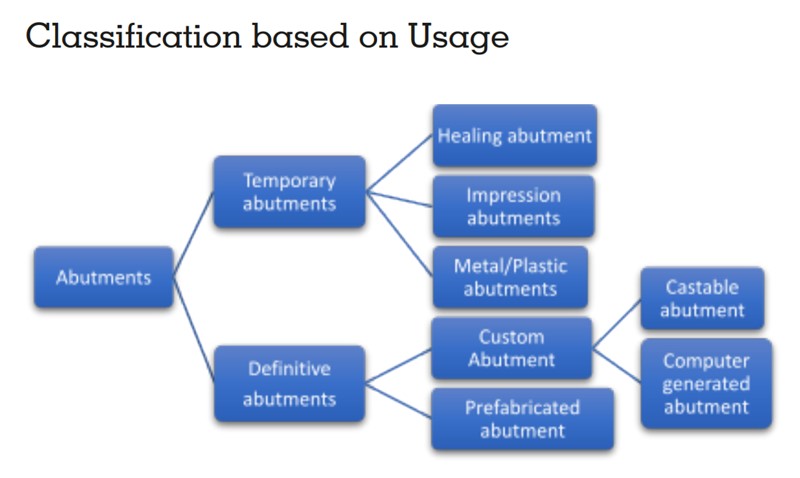
They are used for a definitive period inorder
to shape gingival tissues, helping to create an
emergence profile, establishing esthetics phonetics in the final restoration. They play a major
role in the outcome of the final restoration. 1
The healing abutment
The healing abutment protects the implant platform and aids in preventing soft tissue and bone
growth onto the crestal area. It protects the surgically placed implant from oral fluids and epithelial ingrowth. One stage or 2 stage protocol is
followed whereby the former allows the healing
abutment to be exposed during healing phase
and allows direct accessibility to the implant
platform. The two- stage protocol requires the
submerged implant platform under the soft tissue to be uncovered in a surgical manner.
Impression abutment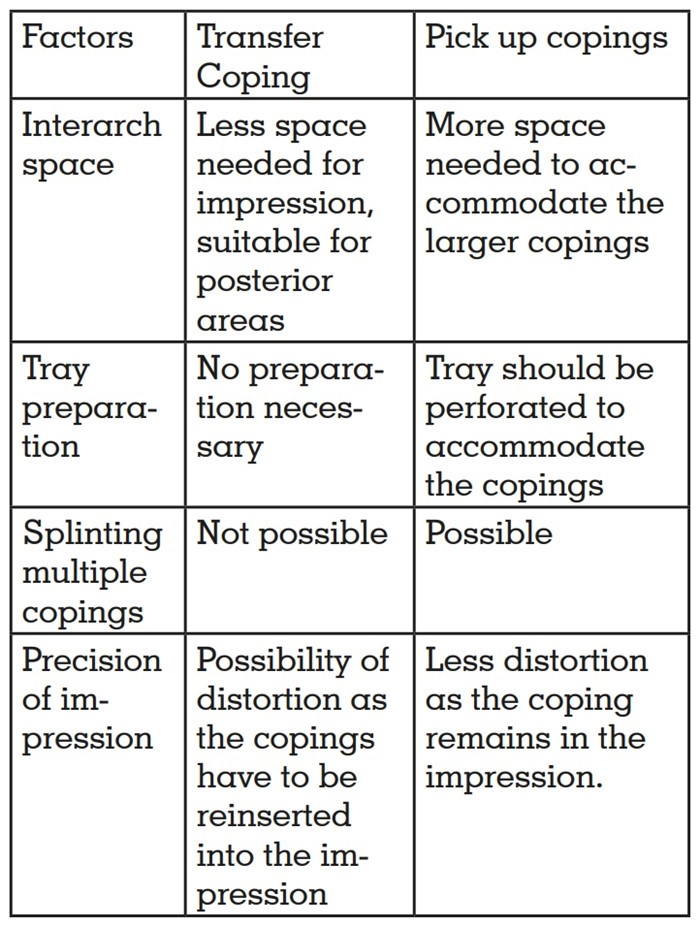
Commonly known as copings, there are two
types based on the clinical scenario. The
Pickup or direct copings for is for the open
tray impression whereas the Transfer or indirect copings is for the closed tray impressions.
Metal or plastic abutments
These abutments are mainly used for provisionalization and mainly help in soft tissue
contouring and establishing occlusion prior
to the final restoration. It can be prefabricated or customised according to the patient
profile.
Prefabricated Abutment
Prefabricated abutments, being manufactured
by implant companies are of varying configurations, may be selected directly by an implant or
fixture level impression or it may be directly selected and a crown fabricated.
Custom Abutment
The custom abutment is suited for more complex
and esthetic areas, can be fabricated in a dental
laboratory or milled by CAD CAM, requires precise impression to be made at the implant fixture
level.
Castable abutments
These are waxed up and customised for the
restorative space. It requires labour intensive procedures like waxing, investing, and
casting with alloys at high temperature.
This makes it costly, time consuming, and
involves more complex laboratory procedures4
Computer-generated abutments
CAD/CAM technology was introduced in the
1980s. It uses data from a computerised tomography scan. The CT images are converted into
data that are recognized by a software.5
It ensures precision which is crucial in implant dentistry for fit, stress distribution, longevity, passivity, and long-term success. 6
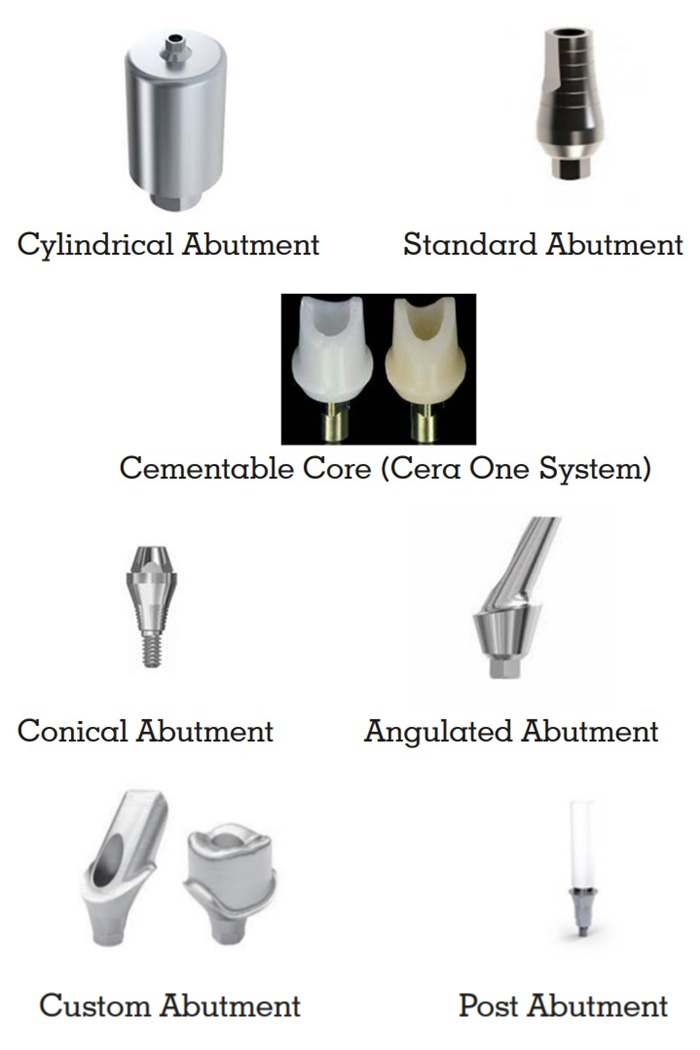
Abutment can be categorised for use with any
hexagonal root form implants
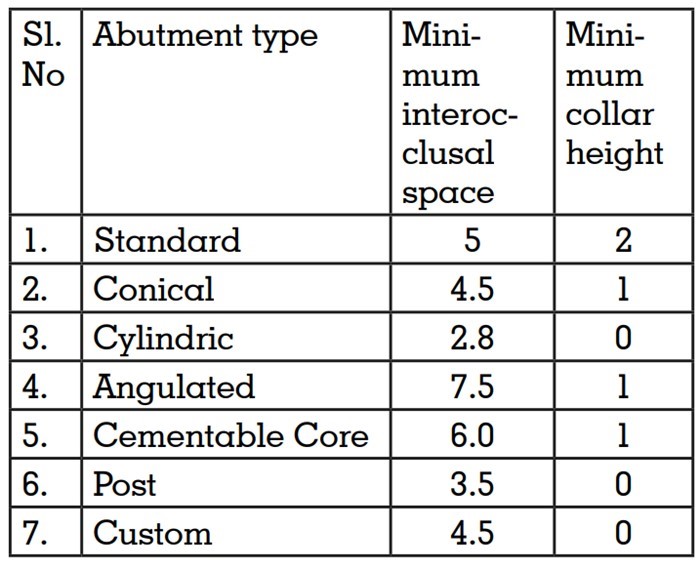
Implant level restoration (2 tier system)
Cylindrical abutment
It is the only implant level (2 tier system) restoration available. Commercially it is known as
UCLA or gold UCLA. It is available with a collar
height less than 1mm and requires an interocclusal space of 3.5 mm.1
Abutment level restoration (3 tier system)
Standard abutment
It varies from 2-8mm of collar height and requires
5mm of interocclusal space. Multiple units can
be placed in non esthetic areas. It is supragingival and easily cleaned.
Conical Abutment (Esthetic zone)
It has a more esthetic emergence profile due to
more subgingival placement. Single or multiple units can be places in esthetic areas. There is a
problem of interproximal tissue collapse into the
abutment due to collar height being uniform.13
Angulated abutment
It is used in cases of angulation and positional
discrepancies. It has a disadvantage of tissue
impingement problem caused by ledge. 14
Cementable Core (Ceraone System)
It is indicated in highly esthetic single tooth
abutments. The screw deforms inside the implant and increases retention.
Post Abutment
It is screwed into the implant or cast and prepped
as tooth in fixed prosthesis. The preparation
is refined intraorally, crown fabricated and cemented over the post.
Custom Abutment
It enhances the esthetic emergence as it can be
customised to match individual cases. The main
drawback is the increased lab cost and orientation problems which occur due to the 6 different
positions in which the abutment is placed.
1) Syncone abutments
Prefabricated telescopic conical abutments having a 4° angulation (SynCone System, Friadent,
Mannheim, Germany). The prefabricated abutments are designed to fit precisely into secondary copings that are placed into the denture’s
base. When compared to bar-retained dentures,
they allow for improved oral cleanliness and
drastically lower the cost of fabricating customized castings.15

2) Multiunit abutments
Multi unit abutments are intended to be connectors between dental implants and multiple
implant screw retained restorations. These are
mainly indicated for multi unit screw retained
restorations. It can either be straight or angulated and be of varying heights from between 1 to
5mm.2
A major advantage is that when the multi unit
abutments are placed at the time of surgery,
they don’t have to be removed for the impression
which aids in preserving the adherent epithelial
and connective tissues. Using a multi unit abutment will also bring the margin of the restoration
closer to the tissue level which can make it much
easier to seat the restoration. 16

3) Digital abutments for scanning
Transferring the ultimate implant position to the
final restoration is the goal of an implant clinician. Implant-supported full-arch frameworks
can be recorded best with digital impressions.
Scan-bodies are typically fastened into implants
in order to create digital impressions.
A scanning abutment is a type of abutment that
is used to transmit data related to the angulation
and position of seated implants. The data is collected with a digital desktop scanner or an intraoral scanner and is extremely accurate. It is important to consider transmission faults brought
on by the usage of scan-bodies.17

4) Zirconia and PEEK abutments
The use of alternative materials for implant abutments were deemed necessary due to gray zone
effect created by Titanium abutments in peri implant marginal mucosa, which reduces patient
esthetics and satisfaction. Zirconia( polycrystalline ceramic material) reduces the greying effect
on the mucosa and promotes adequate esthetics
and durability.
High Performance Polymer (Bio-HPP) are polyetheretherketone (PEEK) based biomaterials,
that have been developed as a promising alternative, is a semi-crystalline linear polycyc thermoplastic that has many advantages including lower hypersensitive and allergic reactions,
radiolucency and it reduces the incidence of artifacts on magnetic resonance imaging.18

5) UCLA abutments
When the UCLA abutment was first introduced
in 1987, its goal was to have the best possible
aesthetics. It also resolves issues with implant
angulation, soft tissue response, limited interocclusal and interproximal distances, and implant
angulation. It is possible to correct an angle of
up to 30 degrees. For cosmetic reasons, tooth
color can be customized, and the healing period
is comparable to that of other abutment materials.8

6) Key solution ( Ks) implant system
KS implant system provides durable stability
for patients and easy access and manipulation
for dentists. With an internal hexagonal connection and 15 degree morse taper. It has enhanced
strength and fracture resistance. The surface of
the KS system is coated with barium, a super-hydrophilic coating that boosts osseointegration
by increasing blood adhesion. The substance
is 100% bioabsorbable and provides excellent
healing efficacy.8

7) Locator Abutments
The locator abutment is a popular choice for
implant retained or implant supported overdenture due to its low level of thickness ( 2.5 mm)
and ability to self align, which can correct upto
40 degree of implant angulation. It provides excellent retention and stability and offers for easy
hygiene maintainance. It can be used in cases of
narrow inter arch space and prevent fracture of
denture base.8

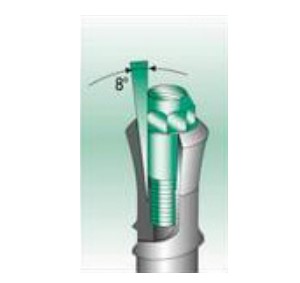
8)Morse Taper abutments
A unique design feature of the Morse taper implant-abutment connection is an internal joint
design between two conical structures. The substantial proclivity for parallelism between the
two structures in the joint space results from this
internally tapered design, which causes a great
deal of friction. It has reduced biofilm accumulation, less periimplantitis when placed supracrestally, Reduced resorption of crestal bone19
9) Platform Switching Abutments
When an abutment is used that is smaller in diameter than the implant platform, this is referred to as platform switching, also known as platform
shifting. The long-term stability and success of
the implant depend on preventing crestal bone
loss, which can be achieved by switching platforms. Additionally, it may increase the amount
of soft tissue surrounding the implant platform,
which will enhance the esthetic end result.19

With an increase in the availability of implant
restorative components, the selection of an appropriate implant abutment for a given clinical
situation has become more challenging. The
implant clinician should select the abutment
during planning of the restoration. The overwhelming number of abutments available become more manageable if they’re categorized
by their properties into certain groups based on
the criteria. The implant abutment connection,
material, retention type, and production techniques of these abutments differ. Since every implant case is unique, clinicians should be able to
recognize the needs of each one and select the
best abutment on the market.