

Rehabilitation of patients with a deep bite is restored either with a tooth-supported fixed prosthesis, implant prosthesis, or by a combination of both. Implant-retained fixed bridges range from limited span to complete arch for dentulous and edentulous jaws. The desire to achieve expected results has in the long-run involved several issues concerning the materials, techniques, and anchorages used. Concerning the types of connection between the implant and restoration, these can be screwed, cemented, or a technique combining both can be implemented. The purpose of this article is to describe an impression technique and its various procedures for the rehabilitation of a patient with a deep bite using a tooth and implant-supported prosthesis.
Key words: deep bite, full arch rehabilitation with implant and tooth-supported prosthesis, esthetic smile, castable abutments, and screw-retained implant prosthesis.
The occlusal vertical dimension (OVD) is defined as
the distance between two selected anatomic points
in a maximal intercuspal position1
. Collapsed
bite occurs in one of the two situations. Firstly,
the patient grinds their teeth aggressively and
reduces the biting surface. Secondly, when enough
teeth are lost and remaining natural teeth and
supporting alveolar bone are unable to withstand
normal biting forces and begin to tip sideways,
resulting in over-closure of the jaws. For evaluation
of the adequacy of this, it is compared with the
physiologic rest position of the mandible2
. When
permanent teeth are missing, a removal partial
denture can never be the solution3
. Rehabilitation
of these cases is done either with a tooth-supported
fixed prosthesis, implant prosthesis, or by a
combination of both. Successful placement of
implant retained prosthesis depends greatly
on the technique and materials used4
. It also
involves the osseointegration of implants that are placed in an ideal position for the fabrication of
prostheses5
. Nowadays the most pleasing smiles
which have vanished due to the loss of teeth,
supporting alveolar bone, and muscle are created
by prosthetic materials6,7. The use of implant-retained fixed bridges ranging from limited span
to complete arch restoration has become a popular
mode of treatment in recent years8,9.
A 30-year-old female reported to the Department
of Prosthodontics and Crown & Bridge willing to
restore her lost smile and teeth. On examination,
it was found that her maxillary canines were
impacted as well as she had faulty fixed bridges
in regions 14 to 17 and 24 to 26 with missing 15 16,
and 25 respectively. The patient also had missing
mandibular posteriors in both quadrants and root
canal treated mandibular anterior. The patient had
a deep bite in the anterior region and collapsed
bite in the posterior region and she wanted to
rehabilitate them. The patient was not willing to
her maxillary central incisors rather she wants
to leave them as it is. A proper case history was
recorded for the patient including noncontributory
medical history, routine blood investigations, and
dental and oral examinations. After clinical and
radiological assessments (Figure1), considering the loss of bone, labial support, and financial
status, it was decided to remove the faulty bridge
and restore the lower posteriors with an implant-supported fixed prosthesis and fixed crowns for
the remaining teeth.

After clinical and radiological assessments
including cone beam computerized tomography,
titanium implants (Adin-dis, Israel) were placed
in locations 34(3.75W/8L), 35(4.2W/6.2L),
36(4.2W/6.2L) in first appointment and locations
44(3.5W/10L), 45(3.5W/10L), 46(4.2W/6.2L),
47(3.5W/10L) at second appointment (Figures 2a,
2b, 2c). The two-staged approach was employed
and implants were left to submerge healing. After
four months of an osseointegration period, healing
abutments were placed.
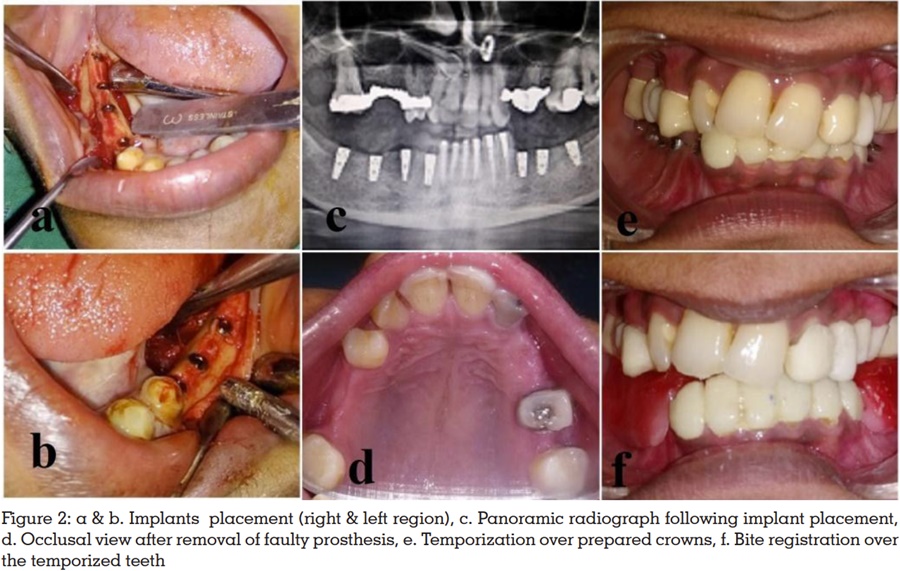
After implant placement, at the first prosthodontic
visit faulty fixed prostheses from 14 to 17 and 24
to 26 were removed. Because of extensive decay
extraction of 24 and endodontic therapy in 14, 22
and 26 were advised (Figure 2d). Tooth preparation
in locations 31, 32, 33, 34, 41 and 42 were done
and temporary crowns were given at raised bite
within the physiological limits. After healing of extracted sites as well as completion of root canal
treatment of desired teeth, fiber post was placed
in 14 and tooth preparations of 12, 14, 17, 22, 26
and 27 were done. Temporary crowns for these
teeth were also given at raised bite within the
physiological limits (Figure 2e). Prior to impression
making of both the arches, the occlusal rim was
made on mandibular posteriors and inserted in
the patient’s mouth to check for the raised vertical
dimension (Figure 2f).
After evaluation of the vertical dimension, the
impression for the maxillary arch was made
with a single-step putty wash technique using a
custom tray. For the impression of the mandibular
arch open tray impression copings were screwed
in the patient’s mouth, and a putty impression
was made with an open stock tray for diagnostic
purposes. After retrieval of the impression implant
analog was placed and cast was poured with type
III dental store and a jig was made with dental
floss and pattern resin over it by screwing the
impression copings with implant analogs. The
jig was examined intra-orally to check for implant
parallelism and transferred to the diagnostic cast.
A new custom tray was fabricated over it for making
final impression. The open tray impression posts
were again tightened in the patient’s mouth and
the final impression was made with a custom
tray using single-step putty wash technique. The
impression was disinfected with 2% gluteraldehyde
solution and sent to the lab along with the castable
abutments for the fabrication of porcelain fused to
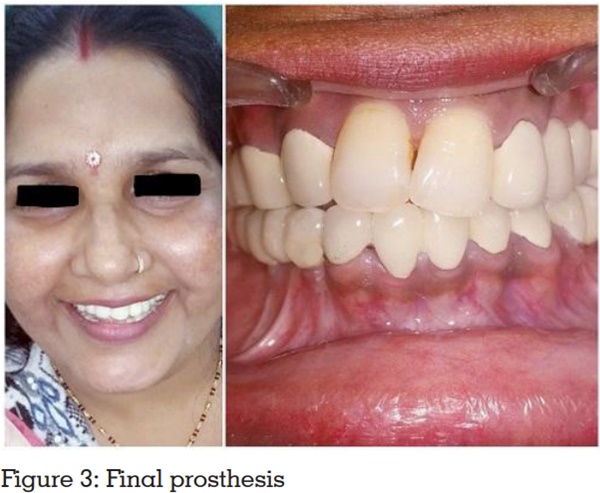
metal prosthesis. The prosthesis fit was verified in
the patient’s mouth. Desired occlusal corrections
were made according to centric, lateral, and
protrusive movements. Group function occlusion
was achieved; the prosthesis was glazed and
luted with Glass Ionomer Cement (Figure 3). The
patient was highly satisfied with her enhanced
smile. Post-operative instructions were given and
regular follow-up appointments were maintained after every 3 months.
Rehabilitation of completely edentulous patients
offers a great challenge to dentists when a lack of
restorative space or other problems exists10,11. In
patients who are periodontically healthy, full mouth
rehabilitation using implant-supported prosthesis
has become a widely accepted treatment option12.
However, various treatment strategies have been
developed for oral rehabilitation13. Implant-supported prostheses are the best treatment option
for restoring difficult situations, which is sometimes
impossible via conventional prosthesis as it fulfills
both functional and esthetic requirements of the
patient14. In 1984, Turner classified the treatment
of a collapsed bite by the amount of loss of VDO
(Vertical Dimension at Occlusion) and available
space to restore it15. In these kinds of cases where
interocclusal space or esthetics is of prime concern,
increasing the OVD becomes inevitable16. His
classification as well as conventional treatment
includes raising the VDO with multiple crown-lengthening procedures has been widely used
to date. However, the etiology for such situations
is multifactorial, clinically controlled trials of
restorative and Prosthodontic approaches are
limited in quality and quantity. Moreover, there is
lack of evidence regarding the long-term outcomes
of the treatment methods as well as materials
which may cause difficulty in clinical decision making17.
According to this clinical report, full mouth
rehabilitation for high aesthetic demands was
carried out effectively by increasing the vertical
dimension of the occlusion as well as correcting
the deep bite utilising temporary crowns following
fixed implant and tooth-supported prosthesis on
the basis of accurate diagnosis.