

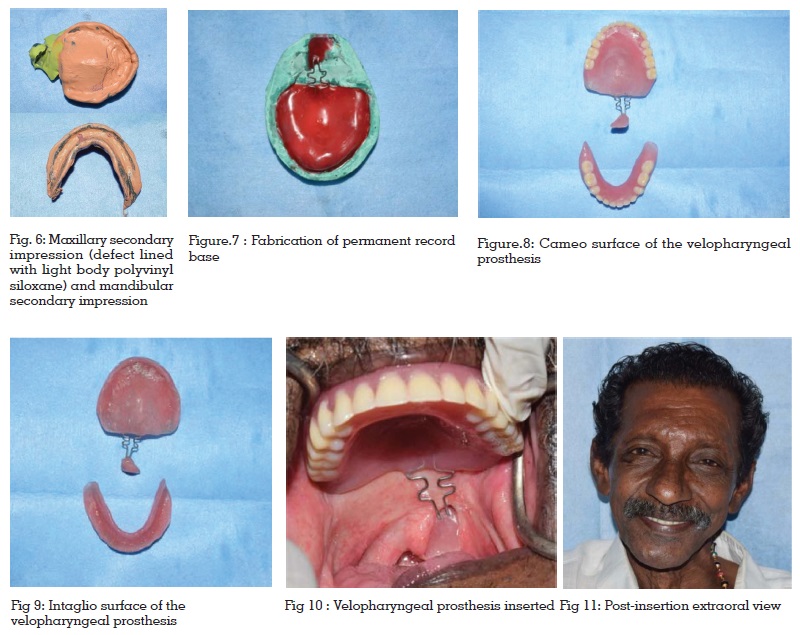
Rehabilitation of partial soft palate defects following surgical resection of neoplastic tissues poses a prosthodontic challenge. The patient may have difficulties in speech and swallowing and nasal regurgitation of food and fluids, which should be dealt with. This case report describes the prosthetic rehabilitation of a completely edentulous patient with an acquired soft palate defect due to surgical resection of oropharyngeal carcinoma. A velopharyngeal obturator combined with a complete denture using resilient orthodontic wires bent into a crib pattern to join the hard and soft palatal parts of the prosthesis were used in the procedure. For obtaining effective nasopharyngeal obturation, the contours of soft palatal defect were carefully recorded. The prosthesis fabricated following proper evaluation and planning has improved the quality of life of the patient.
Key words: Velopharyngeal defect, Velopharyngeal insufficiency, Obturator, Soft palate defect, Speech aid prosthesis.
A rewarding area of Prosthodontics is the
rehabilitation of patients with maxillofacial defects.
The Maxillofacial Prosthodontist contributes to
all facets of patient care, from diagnosis and treatment planning to rehabilitation1. The primary
objective in each case is to construct a prosthesis
which will restore the defect, improve aesthetics
and benefit the morale of the patient2.
Successful rehabilitation of soft palate defects is
a challenging task, especially the restoration of
the velopharyngeal mechanism. Soft palate is the
movable posterior portion of the palate that marks
the beginning of oropharynx. Speech utterance
and other oral activities such as swallowing,
blowing, sucking and whistling are regulated by
the palatopharyngeal or velopharyngeal valving
mechanism. Soft palate defects can be grouped
into congenital, acquired or developmental defects
depending on etiology. Most acquired soft palate
defects result from surgical resection of neoplastic
tissues. In the past, reconstructive surgery was
generally not indicated for patients with acquired
defects because tissue loss is often excessive and
it is required to monitor the tumor site for recurrent
disease. However, the recent advancements
in imaging techniques and improved surgical
expertise have made excellent functional results
for reconstructive surgery in selected patients1.
In cases with high surgical risks and patients
refusing a second surgery, the Prosthetist is
called upon for rehabilitation of maxillofacial
defects. This case report describes a completely edentulous patient with a surgical soft palate
defect rehabilitated by a velopharyngeal obturator
connected to the complete denture by resilient
orthodontic wires bent into a crib pattern.
A 60 year old completely edentulous male patient
reported to the Department of Prosthodontics,
Government Dental College, Trivandrum, with a
chief complaint of nasal regurgitation of fluids
and difficulty in speech. (Fig.1)
On eliciting history, the patient was diagnosed to
have oropharyngeal carcinoma for which surgical
resection of soft palate tumor had been done. He
had also undergone post-surgical radiotherapy
which was completed 8 months before reporting
to our department.
On examination, the patient was completely
edentulous and had a soft palate defect on the
left side due to surgical excision of the tumour
(Fig.2 & Fig.3). Observation of patient’s speech
showed hyper nasality of voice. A complete denture
with a velopharyngeal obturator extending to the
velopharyngeal defect was planned.
The retention, stability and support for the
prosthesis were planned to be obtained from
the bilateral undercuts in the molar regions of
maxillary edentulous ridge and the denture
bearing areas of the edentulous maxilla. The
procedure was explained to the patient and a
written consent was obtained.
Post-insertion instructions were given and a regular
follow-up was advised. The patient was satisfied
with the prosthesis (Fig.11) since there was marked
improvement in swallowing and speech.
Velopharyngeal deficiencies may be classified on
the basis of physiology and structural integrity.
Palatal insufficiency occurs when the hard or
soft palate is of inadequate length (to affect
velopharyngeal closure) but the movement of
remaining tissues is within normal physiological
limits. Palatal incompetence occurs when
velopharyngeal structures are essentially normal,
but the intact mechanism is unable to effect
velopharyngeal closure1. The soft palate should
be properly prepared following tumor ablation
by retaining the movements of the residual
velopharyngeal mechanism so that the defect can
successfully be managed by an obturator or speech
aid prosthesis. Velopharyngeal incompetence
due to neurologic disease or trauma resulting in
impaired motor control can prosthodontically be
managed bypalatal lift prosthesis. The functional
component of the speech aid prosthesis is a
nasopharyngeal extension (“speech bulbs”) that
is shaped to conform to the activity of velopharynx
during speech and swallowing whereas the palatal lift prosthesis reduces hypernasality by
approximating the incompetent soft palate to the
posterior pharyngeal wall3.
In this case report, surgical resection of the left
lateral posterior portion of the soft palate had been
done following the diagnosis of oropharyngeal
carcinoma resulting in a soft palate defect.
Reconstructive surgery was not done and the
patient had been referred to the Department of
Prosthodontics for fabrication of an obturator
prosthesis. An interdisciplinary approach was used
for the treatment of velopharyngeal insufficiency
in this case. A speech pathologist was consulted
and the patient was examined for articulation
errors and inappropriate oronasal resonance
balance4. Traditionally, various types of speech
aid prostheses have been used namely, the hinge
type5, the meatus type obturators5, the palatal lift
prostheses6,7, the palatal stimulators7 and the fixedtype
obturators known as a speech bulbs7. The
general objectives of obturation were to provide
the capability for the control of nasal emission
and inappropriate nasal resonance during speech
and to prevent the leakage of material into the
nasal passage during deglutition8,9. The size and
extent of the defect can affect the functioning of
the prosthesis. Larger the defect, greater is the
difficulty to get adapted to the prosthesis and lesser
the improvement in speech. The case discussed
here involves only soft palate defect. Retention of
the prosthesis is by resilient orthodontic wire of 21
gauge bent into crib pattern extending from the
maxillary denture base. Bilateral undercuts in the
maxillary edentulous ridge were utilised here to
achieve retention. In case of edentulous patients
with both hard and soft palatal defect, achieving
effective retention is very difficult.
To obtain an adequate velopharyngeal closure
during speech and swallowing, functional
moulding of the defect had been done. After
moulding, the final impression was examined
for contact with the pharynx bilaterally and
posteriorly. The functional seal was verified by asking the patient to drink water. The water should
not regurgitate into the nasal cavity when patient
was seated in an upright position. Individuals
with a history of radiation therapy had discomfort
wearing obturator prosthesis due to salivary gland
dysfunction and dry mouth10. Mostly patients had
initial difficulty wearing the obturator due to gag
reflex and choking sensation. Careful explanation
of the causes of reflex and how to control it should
be explained to the patient. Periodic check-up and
adjustments were advised because it is necessary
to monitor the tumor site for recurrent disease and
to accommodate tissue changes in the prosthesis.
Prosthetic treatment along with speech therapy
and counselling are necessary for complete
rehabilitation of patients having partial soft
palatal defects. For such patients who cannot be
treated by surgical reconstruction alone, obturator
prosthesis helps to improve the quality of life. Thus,
an interdisciplinary approach with proper care in
the fabrication of the obturator and training of the
patient demonstrate commendable results.